[ad_1]
A research team in India recently described how the field of proteomics could be pivotal in helping tackle the current 2019 coronavirus (COVID-19) pandemic.

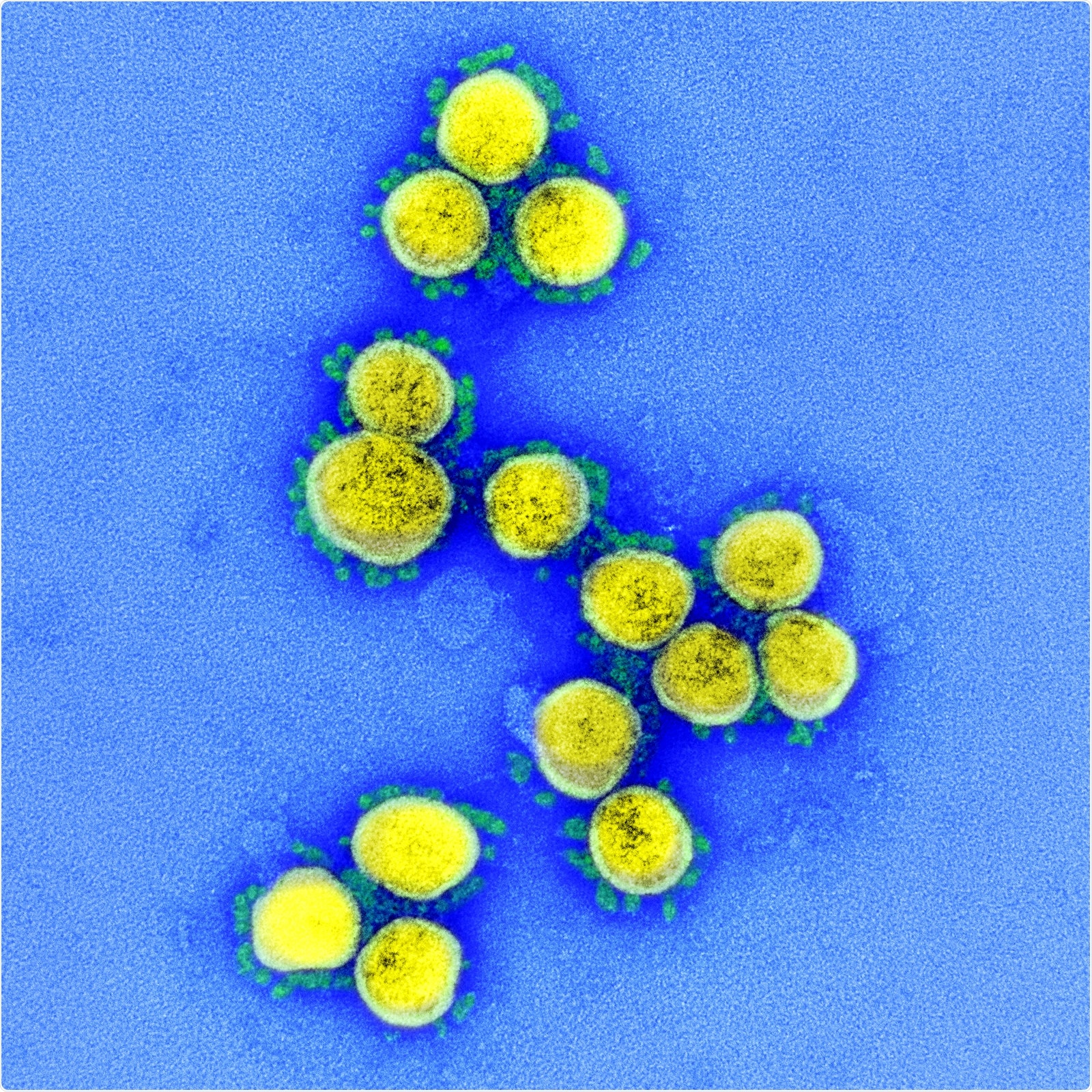
Since the COVID-19 outbreak was declared a pandemic by the World Health Organization (WHO) on 11 Marchth, 2020, scientists have struggled to develop therapies for the prevention and treatment of the causative agent: severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The development of therapeutic and preventive strategies requires an accurate understanding of the role proteins play in the SARS-CoV-2 infection process and in the progression of COVID-19.
The vast field of proteomics is well equipped with the technologies needed to help address this challenge, say Rashmi Rana and colleagues from the Research Department of Sir Ganga Ram Hospital in New Delhi.
In a recent overview published in Journal of Proteins and Proteomics, Rana and the team highlight some of the developments in proteome technologies that have not only accelerated progress in tackling previous coronavirus pandemics, but could also prove invaluable in tackling the current COVID-19 crisis.
Challenges posed by the unprecedented spread of SARS-CoV-2
The new coronavirus SARS-CoV-2 is the most recent addition to a group of six other coronaviruses that can also infect people, including SARS-CoV-1, the agent responsible for the SARS outbreak in 2002-2003.
However, the seemingly unstoppable transmission of SARS-CoV-2 has led to unprecedented global infection and mortality rates that have proved particularly difficult to monitor and address, especially given the large percentage of asymptomatic carriers.
Although most patients exhibit mild or no symptoms, about 20% develop severe illness that can lead to symptoms such as pneumonia and respiratory failure.
“Patients presenting with these clinical manifestations have already progressed to a clinically severe stage and require immediate access to specialist intensive care; otherwise they could die quickly, ”the researchers write. Therefore, it is critical that new approaches are developed that can predict and treat cases that could progress to clinically severe disease, they add.
Such strategies mainly focus on proteins involved in SARS-CoV-2 infection, rather than nucleic acids. However, although many of the technologies available to date are effective in counting differentially expressed genes, they often fail to identify the multiple proteins involved, as well as the functional role these proteins play in the infection and progression of disease.
How can proteomics help?
A wide range of identification and separation techniques can isolate proteins from complex mixtures, facilitating the analysis of protein-protein interactions, patterns of temporal expression and cellular or subcellular distribution, for example.
The most common separation methods are one-dimensional and two-dimensional gel electrophoresis and high-performance liquid chromatography, while mass spectrometry (MS) forms the backbone of protein detection and identification.
Protein identification by MS techniques has overcome the limitations of other proteomic technologies (including 2D gel electrophoresis) that require large amounts of purified proteins for analysis.
The contribution of MS-based techniques so far
MS-based viral peptide detection has previously been used to profile viral proteins that affect the airways.
A study that used matrix-assisted laser ionization and desorption flight mass spectrometry (MALDI-TOF MS) to analyze convalescent sera from SARS patients identified a novel nucleocapsid protein that was subsequently established as the immunogen the main SARS-CoV-1.
Currently, reverse transcription polymerase chain reaction (RT-PCR) is the primary method used to detect viral genes in COVID-19 positive patients. However, the high mutability of SARS-CoV-2 may mean that RT-PCR is not sensitive enough to detect these genes. Furthermore, the technique is low throughput due to its long reaction times.
MS-based detection, on the other hand, can provide quick and easy detection of SARS-CoV-2, even among recovered patients.
One technique, called multiple reaction monitoring mass spectrometry (MRM-MS), detected peptides in the SARS-CoV-2 structural spike protein with 90% sensitivity and 100% specificity among cured patients who tested negative for the virus. by RT-PCR.
Protein microarrays could also help improve diagnostics
Protein microarrays provide another valuable platform for the detection of viral peptides in a protein complex.
In a recent study, an opto-microfluidic detection platform rapidly detected antibodies to the SARS-CoV-2 spike protein in highly sensitive diluted human plasma, a development that could significantly improve diagnosis.
Rana and colleagues say that comparative studies of patients in different stages of SARS-CoV-2 infection are urgently needed to help determine how non-severe or asymptomatic patients progress to severe or life-threatening symptoms.
A recent study used single-molecule array technology for quantitative studies of the SARS-CoV-2 spike protein, S1 spike subunit, and nucleocapsid protein proteome in the blood plasma of COVID-19 patients.
The study, which was the first to detect these SARS-CoV-2 antigens in the blood, revealed that the antigens are associated with disease progression.
What could proteomics mean for the future?
The broad field of proteomics can generate information that leads to a better interpretation of the processes involved in SARS-CoV-2 infection and disease progression.
“For many decades, proteomics has demonstrated its versatility and efficacy for developing new potential drug targets for constantly appearing diseases that pose challenges to humanity,” write Rana and colleagues.
In the context of COVID-19, proteomics can help reveal new biomarkers and define point-of-care procedures that could mean affordable healthcare can be provided closer to the patient’s home environment, they say.
“In this developing world, there is a challenge to more effective care for SARS-CoV-2 and point-of-care testing could play a much more important role here in the future,” the team concludes.
.
[ad_2]
Source link