[ad_1]
Using a number of different monoclonal antibodies, the researchers determined several mutations in the SARS-CoV-2 spike protein that leads to resistance. Understanding these resistant mutations is important for the development of effective therapeutic strategies.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for the COVID-19 pandemic, infects host cells through spike proteins on the surface of the virus. The N-terminal (S1) subunit plays a role in receptor binding and the C-terminal (S2) subunit helps in the fusion of the virus host cell membrane.
S1 receptor binding domains (RBD) bind to human angiotensin 2 converting enzyme (ACE2). SARS-CoV-2 antibodies prevent infection by targeting RBD.
RNA viruses, such as SARS-CoV-2, are present as a swarm of genomic sequences around a central sequence. Variants can escape this swarm in the presence of antibodies or drugs and become resistant.
There are now more than 2,700 mutations identified in the SARS-CoV-2 virus spike protein. There may be several mechanisms for these mutations, such as host adaptation and immune selection during natural infection. Additional mutants could arise with the use of vaccines, therapeutic antibodies and convalescent plasma therapy, which can reduce the effectiveness of these therapies.
Mutations resistant to antibodies
In a prepress document published on bioRxiv* server, researchers at Washington University in St. Louis, Harvard and the Mayo Clinic report on the mutational landscape of resistance in SARS-CoV-2 RBD using a variety of monoclonal antibodies (mAbs).
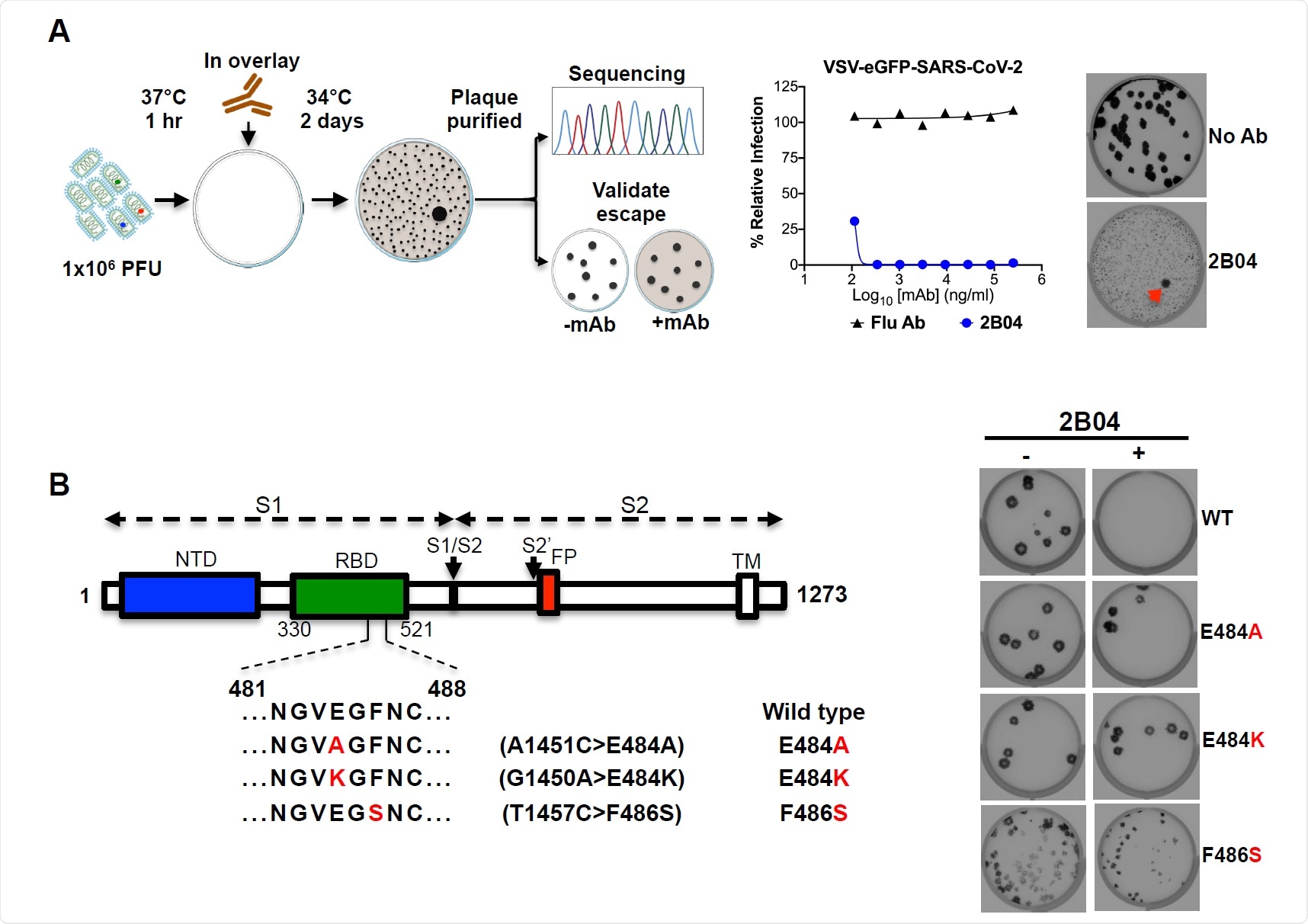
They used a chimeric infectious vesicular stomatitis virus (VSV), a mimic of SARS-CoV-2, where they replaced the glycoprotein with the SARS-CoV-2 spike protein. Using MAb 2B04, the authors determined that the non-neutralized SARS-CoV-2 variants had mutations in RBD related to residues involved in ACE2 binding.
Further tests with nine other mAbs revealed a similar result. For mAb 2H04, resistance mutations were present outside the ACE2 binding site, on the side and on the base of the RBD. This suggests that virus neutralization may take place via alternative attachment factors.
Several resistance mutations were common among the different mAbs tested, suggesting that they represent important antigenic sites on RBD.
The resistance mutations resulting from the different mAbs made them resistant to the other mAbs in the chosen mAb matrix. The replacements in S477 and E484 resulted in ample resistance, while the replacements in many other sites resulted in resistance to more than one mAb.
Human soluble ACE2 receptors, which are not attached to cells and can compete with those on the host cell to bind to the virus, are another strategy being studied to fight the virus. The authors tested the resistance of Vero E6 cells to human and murine soluble ACE2. Soluble ACE2 in humans neutralized all escape mutants, although some mutations required higher ACE2 concentrations to neutralize.
The authors also used serum from four convalescent COVID-19 patients to test whether serum antibodies neutralized escape mutant viruses. They found many mutations resistant to neutralization by the sera. In particular, the mutation at residue E484 was resistant to all four sera, suggesting that it is an important neutralizing epitope. However, substitution at this location was quite rare and was found in only about 0.05% of the sequenced strains.

VSV-SARS-CoV-2 escapes mutant isolation. (A) Schematic of the escape mutant selection experiment. 2B04 and a control anti-influenza mAb were tested for neutralizing activity against VSV-SARS-CoV-2. The added 2B04 concentration in coverage completely inhibited viral infection (middle panel). The data are representative of two independent experiments. Plaque analyzes were performed to isolate the escape mutant VSV-SARS-CoV-2 on Vero E6 TMPRSS2 cells (red arrow indicated). Plate analysis with 2B04 in the overlap (lower plate in the right panel); plaque test without Ab in the overlap (upper plaque in the right panel). The data are representative images from three independent experiments. (B) Schematic of the S gene, which underwent Sanger sequencing to identify mutations (left panel). For validation, each VSV SARS-CoV-2 mutant was tested in plaque assays with or without 2BO4 in the Vero cell overlay (right panel). Representative images of two independent experiments are shown.
Resistant mutations found in human virus isolates
The authors also tested additional mutations, adding up to 48 different escape mutants. The team also investigated whether any of these mutants are present in human SARS-CoV-2 isolates by compiling the available genomic sequences of the virus and comparing them to the genomic sequence of the mutants. They found that 27 of the 48 mutations are circulating in humans, with the most frequent mutation observed being D614G, observed in 86% of isolates.
The substitution for S477N, which conferred resistance at some level in all mAbs, was the second most abundant variant in human isolates.
The authors also note some limitations of the study. Although VSV is an effective imitation of the SARS-CoV-2 virus, 27 escape mutants have been found in human isolates of the virus alone. They also note the few human sera tested. Multiple human serum samples can help determine the extent of neutralization and escape the mutants present.
If such changes in the virus occur after vaccination, they could limit the effectiveness of the treatment. “The relatively low genetic barrier to resistance combined with knowledge of the presence of relevant substitutions in clinical isolates suggests that effective mAb therapy is likely to require a combination of at least two neutralizing antibodies,” the authors write. Determining residues resistant to specific antibodies could help select combinations based on non-overlapping resistant mutations.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be considered conclusive, guide health-related clinical practice / behavior, or treated as consolidated information.
.
[ad_2]
Source link