
[ad_1]
Credit: Public Domain Unsplash / CC0
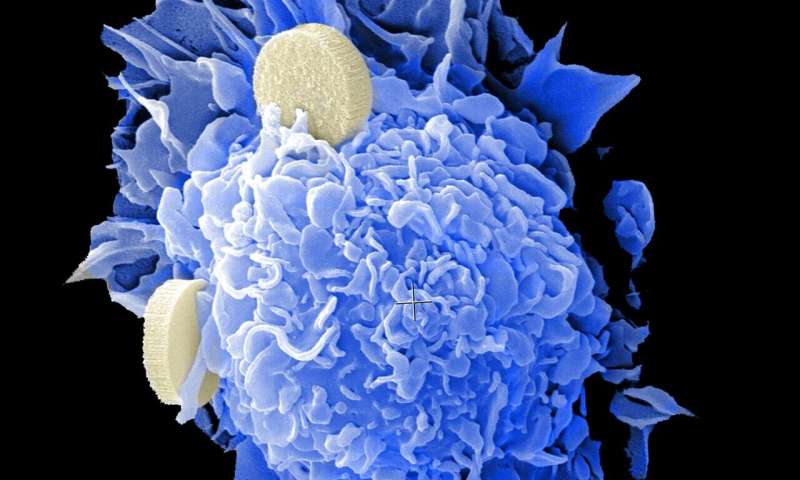
Treatments that use the immune system to fight cancer have greatly improved outcomes for some people with cancer. Scientists are learning more about why some people respond so much better than others to these drugs.
One major factor is something called tumor mutation load (TMB) – the number of DNA changes a tumor has. Studies by researchers at Memorial Sloan Kettering and elsewhere have shown that tumors with high TMB tend to respond better to immune checkpoint inhibitors. In 2017, the U.S. Food and Drug Administration approved the checkpoint inhibitor pembrolizumab (Keytruda) for the treatment of cancers with a type of genetic defect called mismatch repair deficiency (MMR).
MMR is one of several DNA repair pathways that cells use to correct errors in DNA. Mutations in this pathway lead to defective DNA repair and thus to higher TMB. Alongside MMR, the most commonly mutated DNA repair pathway is called homologous recombination, which repairs double-stranded breaks in DNA (in other words, when both sides of the DNA “ladder” are broken). The genes of cancer predisposition BRCA1 is BRCA2 belong to this path. When they are mutated, DNA damage builds up and increases the risk of developing several types of cancer, including breast, ovarian, prostate and pancreatic cancers.
MSK scientists are now reporting that mutations in one BRCA gene, but not the other, produce tumors that respond well to immunotherapy.
“When we started this work, we thought tumors with both types of homologous recombination deficiency would respond to immunotherapy based on the high mutation load,” says physician-scientist Nadeem Riaz. “But we found that instead BRCA2– mutated tumors responded much better than BRCA1 tumors. “
The unexpected results, which were published on November 16 in the journal Cancer Nature, it can have implications for the types of treatments people are subjected to BRCA2 mutations should be considered.
A surprising divergence
The researchers made their findings using both human data and mouse models. When they compared tumor mutations and clinical information from patients treated with immunotherapy at MSK, they found a direct correlation between the mutations BRCA2 and better survival after treatment.
To confirm that this correlation was more than just a chance discovery, they created genetically modified mouse models of BRCA1– is BRCA2– mutant breast and colorectal cancers. In both cases, they found that only the BRCA2– mutant tumors responded to treatment with checkpoint inhibitors.
As well as being surprising, the results were a bit counterintuitive.
“Five years ago, people probably would have thought BRCA1 it would have been the most immunogenic tumor, “says Dr. Riaz.” This is due to the two types, BRCA1-Mutant tumors tend to have more immune cells within them. It might be expected that having more immune cells means a better response to immunotherapy. But in fact, it was the file BRCA2– mutant tumors that showed the best response “.
Self BRCA1 is BRCA2 they are both involved in homologous recombination and both lead to a higher TMB, because it is only the BRCA2-mutants that appear to respond to immunotherapy?
According to the study authors, it may have to do with the type of mutations each produces. Mutant BRCA2produces smaller deletions in the DNA sequence, for example by removing a DNA base “letter”. These mutations shift the reading frame of genes and change the way the DNA sequence is translated into proteins. Imagine the gene is a phrase that says, “I like chocolate ice cream”. Deleting a DNA letter could change the sentence to “I like hocolatei cec ream”. The immune system detects these erroneous proteins as foreign and attacks the cells that contain them. In reverse, BRCA1 it creates several types of mutations, which are not so easily detectable by the immune system.
Jorge Reis-Filho, physician-scientist of the MSK Department of Pathology and collaborator of the Cancer Nature study, says the findings underscore the importance of testing hypotheses. “Sometimes we think we know biology and know what to expect, but when we investigate in detail using the right tools, the results surprise us,” he says.
“Often it’s not what we don’t know that gets us into trouble, it’s the things we think we know for sure that can lead us astray,” he adds.
Make treatments more precise
The new publication is the first to emerge from the Precision Radiation Oncology Initiative, led by Dr. Riaz. Created by the chairman of MSK’s oncology radiotherapy department, Simon Powell, the initiative aims to make radiation a type of targeted therapy when used in conjunction with other treatments such as immunotherapy. Since radiation damages DNA and forces cells to use their DNA repair pathways to repair the damage, the DNA repair defects that cancer cells often have can be exploited against them.
Although these new findings need to be confirmed by others and validated in clinical trials, they suggest that people with BRCA2-Mutant tumors may be considered enrolling in immunotherapy clinical trials. Several studies are currently enrolling people with BRCA-mutant tumors.
In search of the “distinctive” causes of BRCAness in breast cancer
Robert M. Samstein et al. Mutations in BRCA1 and BRCA2 differentially affect tumor microenvironment and response to checkpoint blockade immunotherapy, Cancer Nature (2020). DOI: 10.1038 / s43018-020-00139-8
Provided by Memorial Sloan Kettering Cancer Center
Quote: For people with certain BRCA mutations, immune activation could be a promising treatment (2020, Dec 1) retrieved Dec 2, 2020 from https://medicalxpress.com/news/2020-12-people-brca- mutations-immune-treatment .html
This document is subject to copyright. Aside from any conduct that is correct for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.
[ad_2]
Source link