[ad_1]
British and American researchers have conducted an experiment that shows, in mice, that the microbiota drags certain immune cells before they migrate to a specific part of our brain.
You will also be interested
[EN VIDÉO] Interview: the intestinal microbiota, an essential ally of the immune system The gut microbiota brings together all the microbes present in our gut. It allows a good functioning as well as a certain protection of the colon. Gerard Eberl, head of the Microenvironment and Immunity Unit at Institut Pasteur, tells us more during this interview.
No, your immune cells aren’t lifting the dumbbells and yours yet microbiota it is not divided into a cardio area on the one hand and weight training on the other. However, a recent study appeared in the journal Nature is transmitted by National Health Institute (NIH) in a press release, shows that some immune cells, plasmacytes, which secrete in particular immunoglobulins A (IgA) partially housed in the dura mater, more precisely inside the meningeal sinuses, first do a small training course in the microbiota.
Gut, brain and immunity
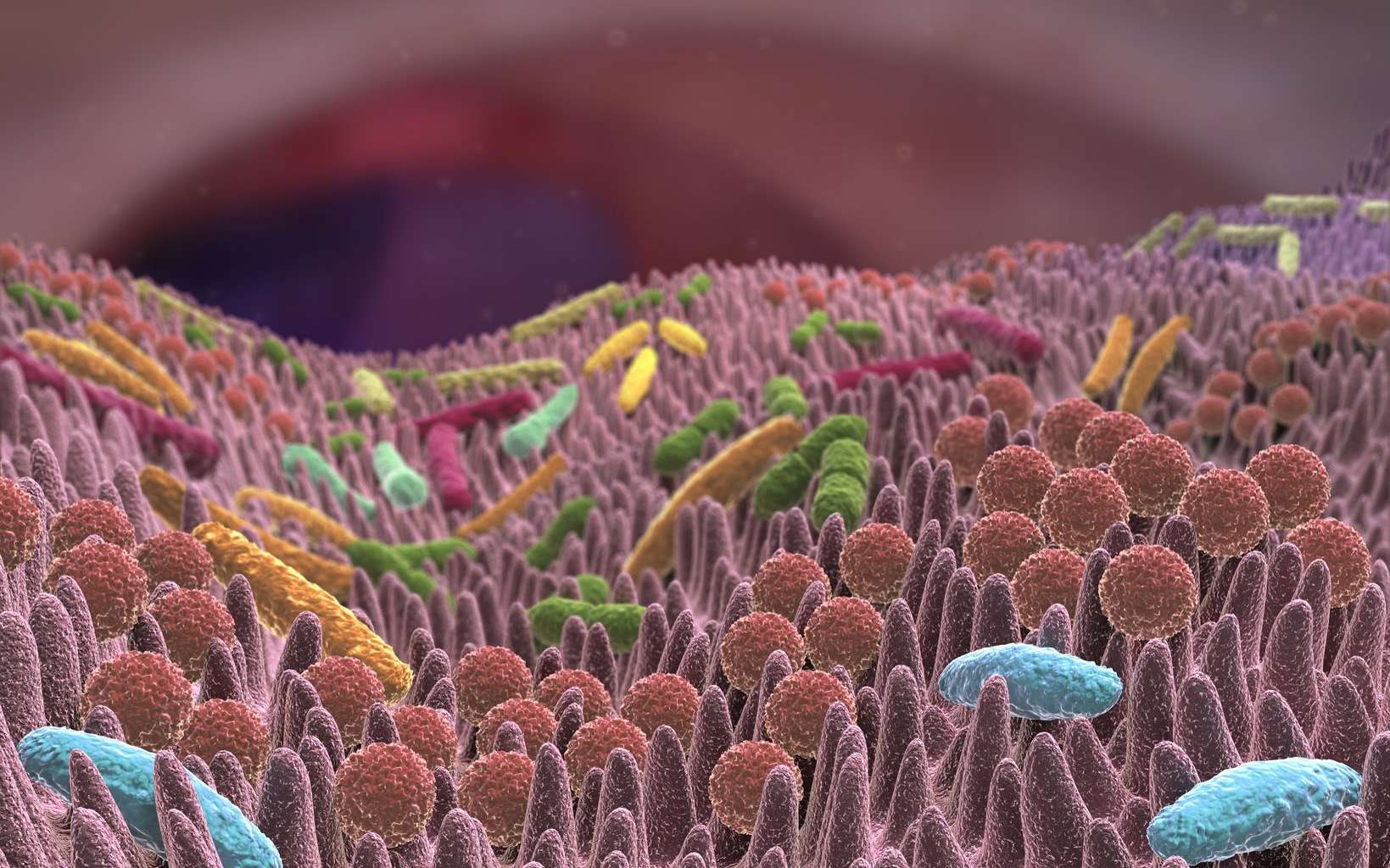
Our instincts are a key organ for our immunity. For mucous sees an army of pathogens potentials every day. In addition to its anatomical barrier – the intestinal barrier – it is a place where many immune cells andantibody, in particular IgA which play a crucial role inimmunity mucous membranes.
” There are two forms of IgA: a circulating monomeric form and a secreted dimeric form. 3 to 5 grams of IgA are secreted in the light intestine each day, which accounts for about 15% of the total immunoglobulin production. The dimeric form is produced by plasma cells (which are lymphocytes B differentiated) in the intestinal mucosa. It binds to a receptor in enterocytes (the cells of the intestine) and is then secreted into the lumen. These protein they are crucial in immune tolerance. In particular, they make it possible to modulate the quantities of bacteria commensals and are an immune barrier against potential pathogens “, explains Filipe De Vader, a researcher at the National Center for Scientific Research (CNRS) who did not participate in the study.
The results of the experiment mentioned above enrich the knowledge in the field of neuroimmunology, more precisely in its links with the intestinal mucosa and the microbiota. In this precise field, most of the results are obtained using models of axenic mice, that is, mice without microbiota. ” What we already knew from the Axenic mouse models is that they have a higher permeability of blood-brain barrier and that the operation of their microglies, the macrophages(immune cells that “eat” pathogens, ed) of brain, is faulty “, says Filipe De Vader.
The microbiota “trains” our plasma cells
In this experiment, the scientists looked at what types of immune cells they were located in our meningeal sinuses, because it is one of the rare, particularly permeable areas of our brain. Curiously, there are plasma cells that produce our little IgA, among other things. Surprised by their results, our experimenters decided to conduct the investigation. They compared the amount of IgA present in meninges from axenic mice and healthy mice.
What they found was that the axenic mice lacked IgA in their meninges. On the other hand, and this is where the experience is bluffing, when we transplant a healthy microbiota into these mice, the IgA network in the meninges is restored. In this phase of the experiment the importance of the microbiota is highlighted. However, it is still unclear where these cells come from.
To find out, the researchers sequenced the IgA present in the meninges and compared their sequence ADN IgA present in the intestine. The similarity of the sequences leaves no room for doubt: these cells in fact come from the intestine. These results therefore demonstrate the experience of the animal model e sequencing in support of that the intestine is a privileged place where the IgA producing cells come to “train” before migrating into the meninges.
” According to this study, the meninges contain plasma cells that secrete IgA. They are found around the sinuses which contain capillaries which are said to be fenestrated, that is, with great permeability; which can potentially allow pathogens to enter the brain. What appears to be happening is that these cells would spend time in our gut to expand theirs spectrum IgA production before accession, through blood circulation, meningeal sinuses. How do these cells know they have to “Stop” in the brain? The question is open ” develops Filipe.
To the intestine and beyond
In their study, the scientists also showed that a mushroom it could easily infiltrate the brains of mice if their IgA production in the meninges were impaired. Likewise, they showed that plasma cells in the meninges do not wait to be exposed to a pathogen to be active. They are constantly anticipating its occurrence. Finally, when the mice are put under antibiotic therapy, we see a file exhaustion the number of IgA in the meninges. The authors therefore suggest that what is known to alter the microbiota (migration, diet change, etc.) can potentially alter the IgA response and increase susceptibility to infections for a short time.
For Filipe De Vader, it is still a bit early for these kinds of claims: ” We know that intestinal infections greatly alter our microbiota, but otherwise it seems to me that little data exists on the matter. What is particularly interesting in this study is that the gut’s immune cells could first, imagine local, move to protect another organ. “ All this paves the way for other hypotheses and other experiments, the results of which will perhaps shock our view of immunity and the relationships our immune cells have with all of our organs.
Do you care what you just read?
.
[ad_2]
Source link