
[ad_1]
Vitamin D is known to have many virtues for human health. Recently, it has been mentioned for its ability to strengthen the immune system and thus limit severe forms of COVID-19. Scientists now give it another power: Vitamin D supplementation could reduce the risk of developing advanced (metastatic or fatal) cancer.
Vitamin D is a fat-soluble vitamin, synthesized by the body under the action of solar radiation. This endogenous origin also explains why, in our latitudes, a good number of individuals have vitamin D deficiencies in winter, when the sun is scarce. To a lesser extent, it can also be provided by food, mainly fish liver oil, so-called fatty fish (salmon, herring, sardines, mackerel, tuna, etc.) and dairy products. According to the National Agency for Food, Environmental and Occupational Safety, the nutritional reference for the population is 15 µg / day for an adult.
This vitamin plays several important roles in the body. In particular, it contributes to the absorption of calcium and phosphorus by the intestine, thus ensuring the maintenance of a sufficient level of calcium. As a result, it ensures good mineralization of the skeleton and joints, effective muscle contraction, as well as good nerve transmission. It is also involved in hormonal regulation and the activity of immune cells. And for several years, scientists have been trying to prove its action on cancer cells.
No influence on the incidence rate
Previous studies have shown that people living near the equator, where sun exposure is greatest – and thus promotes vitamin D production – have lower incidence and death rates for some cancers. Similarly, in experiments with cancer cells in vitro and in mice, vitamin D has been shown to slow cancer progression; reduced the invasiveness of the tumor and its propensity to metastasize.
However, clinical trials in humans have not been able to categorically corroborate these findings. Two years ago, in fact, the American study VITAL aimed at examining the action of vitamin D and omega-3 on the body, revealed that vitamin D does not reduce the overall incidence of cancer. This study was conducted over a five-year period; included more than 25,000 participants, aged 50 and over, who had no cardiovascular disease or cancer at the time of recruitment.
This clinical study aimed to evaluate the independent effects of vitamin D and omega-3 supplements, as well as the synergy between these two nutrients. Participants were then divided into four groups, each receiving all or part (or none) of these supplements: vitamin D (2000 IU per day) + omega-3 (1 g per day), vitamin D + placebo. , omega-3 3 + placebo, therefore only placebo. The primary endpoints were major adverse cardiovascular events and cancer incidence.
The results showed no differences between the groups regarding cancer rates. Conversely, the figures suggest that vitamin D could reduce the risk of death from cancer. Researchers at Brigham and Women’s Hospital then investigated this potential link between taking vitamin D supplements and the risk of developing metastatic or fatal cancer.
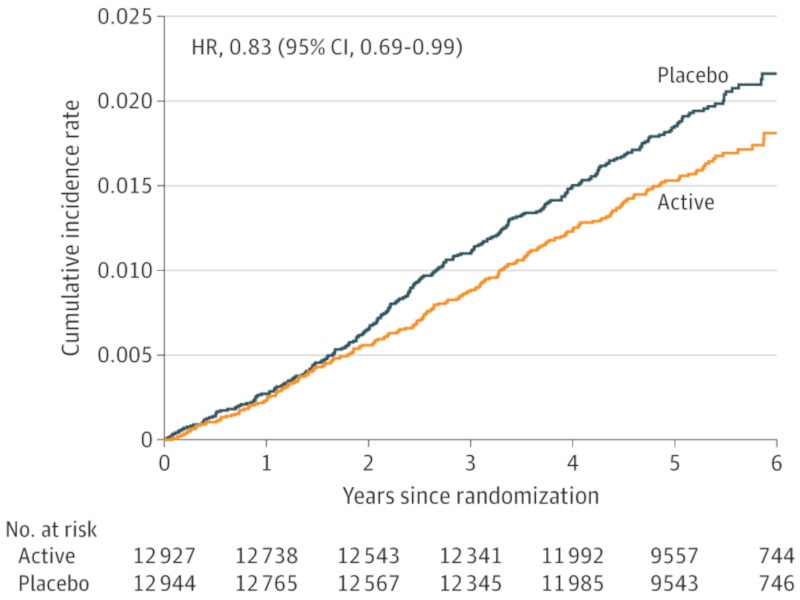
In this new analysis, based on data from the VITAL study, vitamin D appears to be associated with an overall 17% reduction in the risk of advanced cancer. Better still: considering only data from participants with a normal body mass index (BMI), the risk reduction rises to 38%. Body mass would be a factor influencing the action of vitamin D.
An action conditioned by the BMI
Paulette Chandler, a physician and epidemiologist with Brigham’s Division of Preventive Medicine, and her colleagues decided to specifically look at the reduction of cancer deaths and the development of severe cancer in participants with and without drugs. Vitamin D supplements. They also analyzed the potential influence of different BMI categories (normal, overweight and obesity) on the action of this vitamin.
Of the 25,871 participants in the VITAL study, 1,617 were diagnosed with invasive cancer (breast, prostate, colorectal, lung, etc.) within the next five years. Of the approximately 13,000 participants who received vitamin D, 226 were diagnosed with advanced cancer; the number rises to 274 for the group that received the placebo. Furthermore, of the 7,843 participants with a normal BMI (less than 25) who took vitamin D, only 58 were diagnosed with advanced cancer (compared with 96 in the placebo group).
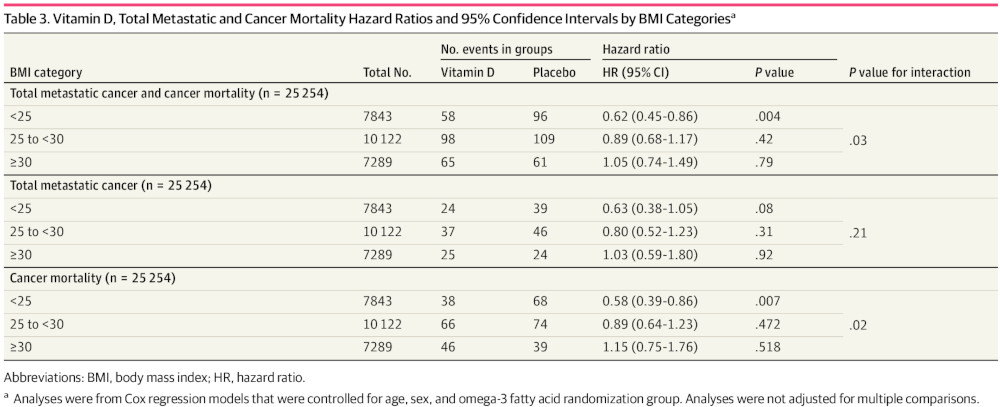
The results of the BMI could be due to chance. However, there is previous evidence of the impact of body mass on the action of vitamin D. Randomized studies to analyze the impact of vitamin D on type 2 diabetes have found better action of vitamin D. vitamin D in people of normal weight; in obese people, however, vitamin D did not show any particular efficacy. Due to the volumetric dilution, people who are overweight or obese may need higher doses to benefit from it.
Additionally, other studies in humans and animals have shown that immune function is impaired in obesity. Obesity has therefore been associated with chronic inflammation and systemic deregulation of natural killer cell function. This inflammation could decrease the effectiveness of vitamin D by reducing the sensitivity of the receptors for this vitamin or by changing its signaling.
Vitamin D deficiency is common in cancer patients; one study reported failure rates of up to 72%! Based on these new findings and previous studies on the subject, Chandler supports the idea that vitamin D supplementation can prevent metastatic cancer. Although the effects of this vitamin have been modest, supplementation at the levels studied is far less toxic and less expensive than many current cancer therapies. The specialist adds that it would be interesting to conduct a complementary study to more precisely analyze the influence of BMI.
Source: JAMA Network Open, P. Chandler et al.
Source link