[ad_1]
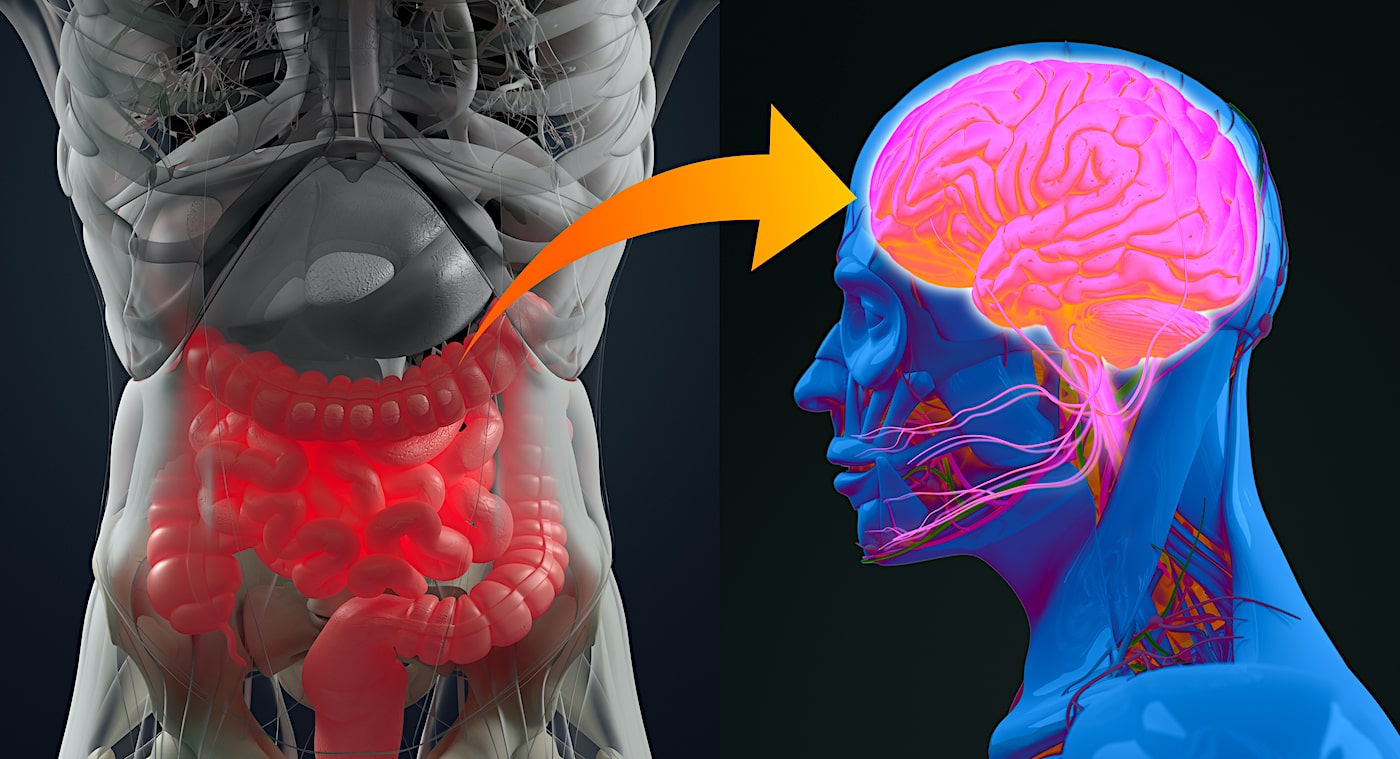
Dementia, when it is not caused by Alzheimer’s disease, is not necessarily of concern for the vital prognosis and mainly concerns the comfort of life of the patient and those around him. Unfortunately, however, the most common cause of dementia is Alzheimer’s disease. Still incurable and fatal in its final phase, it affects nearly a million people in Europe. In recent years, the scientific community has proposed that the gut microbiota plays a key role in the development of the disease, without fully understanding it in detail. Recently, researchers confirmed and provided more details on this link.
A team from the University of Geneva (UNIGE) and the University Hospitals of Geneva (HUG) in Switzerland, in collaboration with the National Research and Treatment Center for Alzheimer’s disease and Fatebenefratelli of Brescia (Italy), University of Naples and the Research Center IRCCS SDN, confirm the correlation between an imbalance of the intestinal microbiota and the development of amyloid plaques in the brain, which are at the origin of the neurodegenerative disorders characteristic of Alzheimer’s disease.
The proteins produced by certain intestinal bacteria, identified in the blood of patients, could in fact modify the interaction between the immune system and the nervous system and trigger the disease. The results, published in Journal of Alzheimer’s Disease, allow to consider new preventive strategies based on the modulation of the microbiota of people at risk.
The research laboratory of neurologist Giovanni Frisoni, director of the HUG Memory Center and professor of the Department of Rehabilitation and Geriatrics of the UNIGE Faculty of Medicine, has been working for several years on the potential influence of the intestinal microbiota on the brain, and more specifically on neurodegenerative diseases. ” We have already shown that the composition of the gut microbiota in patients with Alzheimer’s disease has changed compared to people who do not suffer from these disorders. “, He explains. ” Their microbiota has in fact reduced microbial diversity, with an over-representation of some bacteria and a sharp decrease in other microbes. Furthermore, we also found an association between an inflammatory phenomenon detected in the blood, some intestinal bacteria and Alzheimer’s disease; hence the hypothesis we wanted to test here: can inflammation in the blood be a mediator between the microbiota and the brain? “.
Intestinal bacteria and the immune system
Gut bacteria can affect the functioning of the brain and promote neurodegeneration through several pathways: they can influence the regulation of the immune system and, consequently, modify the interaction between the immune system and the nervous system. Lipopolysaccharides (proteins located on the membrane of bacteria that have pro-inflammatory properties) have been found in the amyloid plaques and around the brain vessels of people with Alzheimer’s disease. Furthermore, the intestinal microbiota produces metabolites – in particular some short-chain fatty acids – which, having neuroprotective and anti-inflammatory properties, directly or indirectly influence the functioning of the brain.
” To determine whether inflammatory mediators and bacterial metabolites are linked between the gut microbiota and amyloid pathology in Alzheimer’s disease, we studied a cohort of 89 people aged 65 to 85. Some suffered from Alzheimer’s or other neurodegenerative diseases that caused similar memory problems, while others had no memory problems. », Reports Moira Marizzoni, researcher at the Fatebenefratelli Center in Brescia and first author of this work. ” Using PET imaging, we measured their amyloid deposition, then quantified the presence in the blood of various markers of inflammation and proteins produced by gut bacteria, such as lipopolysaccharides and short-chain fatty acids. “.
An obvious correlation
” Our findings are indisputable: some bacterial products of the gut microbiota are related to the amount of amyloid plaques in the brain », Explains Moira Marizzoni. ” Indeed, elevated blood levels of lipopolysaccharides and some short-chain fatty acids (acetate and valerate) have been associated with the two large amyloid deposits in the brain. Conversely, elevated levels of another short-chain fatty acid, butyrate, have been associated with less amyloid disease. “.
This work therefore provides evidence of an association between certain intestinal microbiota proteins and cerebral amyloidosis from an inflammatory phenomenon in the blood. Scientists will now work to identify specific bacteria, or a group of bacteria, involved in this phenomenon.
This discovery paves the way for potentially innovative prevention strategies. For example, administering a bacterial or prebiotic cocktail to feed the “good” bacteria in the gut could be a preventative treatment idea. ” However, we shouldn’t rejoice too soon Says Frisoni. ” Indeed, we must first identify the strains of this (bacterial) cocktail. Secondly, a neuroprotective effect could only be effective at a very early stage of the disease, from a prevention rather than a therapy perspective. However, early detection remains a major challenge in the management of neurodegenerative diseases, as protocols need to be developed to identify high-risk individuals and treat them well before detectable symptoms appear. “.
Source: Journal of Alzheimer’s Disease
Source link