[ad_1]
How many people have died from influenza and COVID-19 pandemics
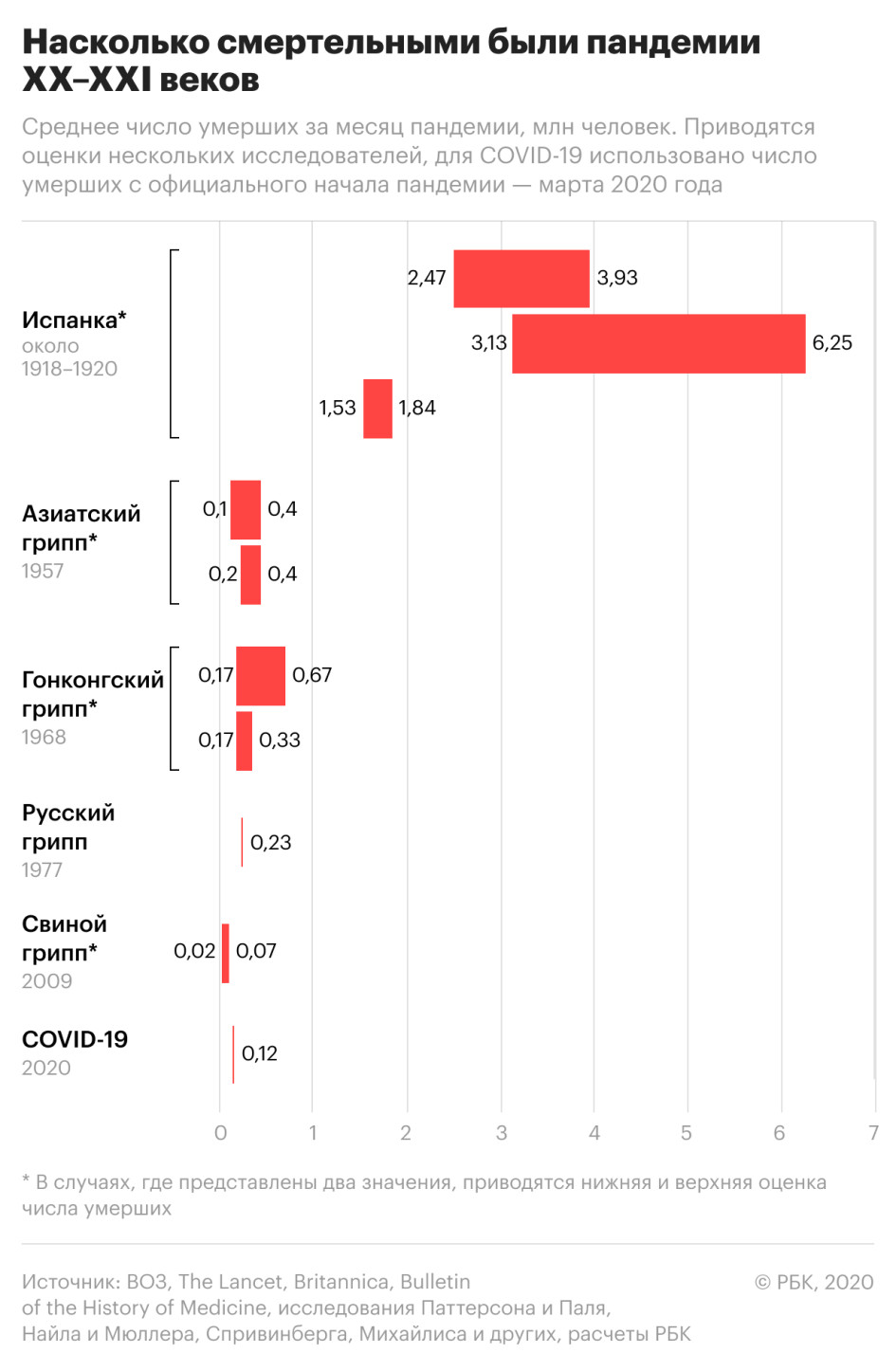
If we analyze the data on the number of deaths from pandemics over the past 100 years, calculating how many people died on average per month with each of them, the most deadly will be the Spanish flu, the so-called Spanish flu, which began in the spring of 1918 and lasted two years. According to various estimates, 17.4 million to 100 million people died, i.e. up to 6.3 million people died every month. The scale of the disaster complicated the postwar years and the lower level of medicine.
Read on RBC Pro
The upcoming influenza pandemics in terms of death toll have turned out to be much smaller in size and may be related to one another to some extent. The last one before COVID-19 was the swine flu pandemic. The influenza A (H1N1) virus was first detected in April 2009 in Mexico and within a few weeks it spread around the world. According to official WHO data, the pandemic has caused the deaths of 18.5 thousand people. However, the figures were recalculated and concluded that there are many more victims – from 152,000 to 575,000.
New restrictions due to COVID-19 around the world. the same thing

Thus, by the highest estimate, this virus killed an average of 70,000 people per month. In August 2010, the WHO announced the transition of the disease to the post-pandemic stage. Therefore, the pandemic lasted 15 months.
The COVID-19 pandemic has been ongoing for eight months (since the WHO announcement) and no one can predict how long it will last. More people died during this period than during the 2009-2010 swine flu surge.
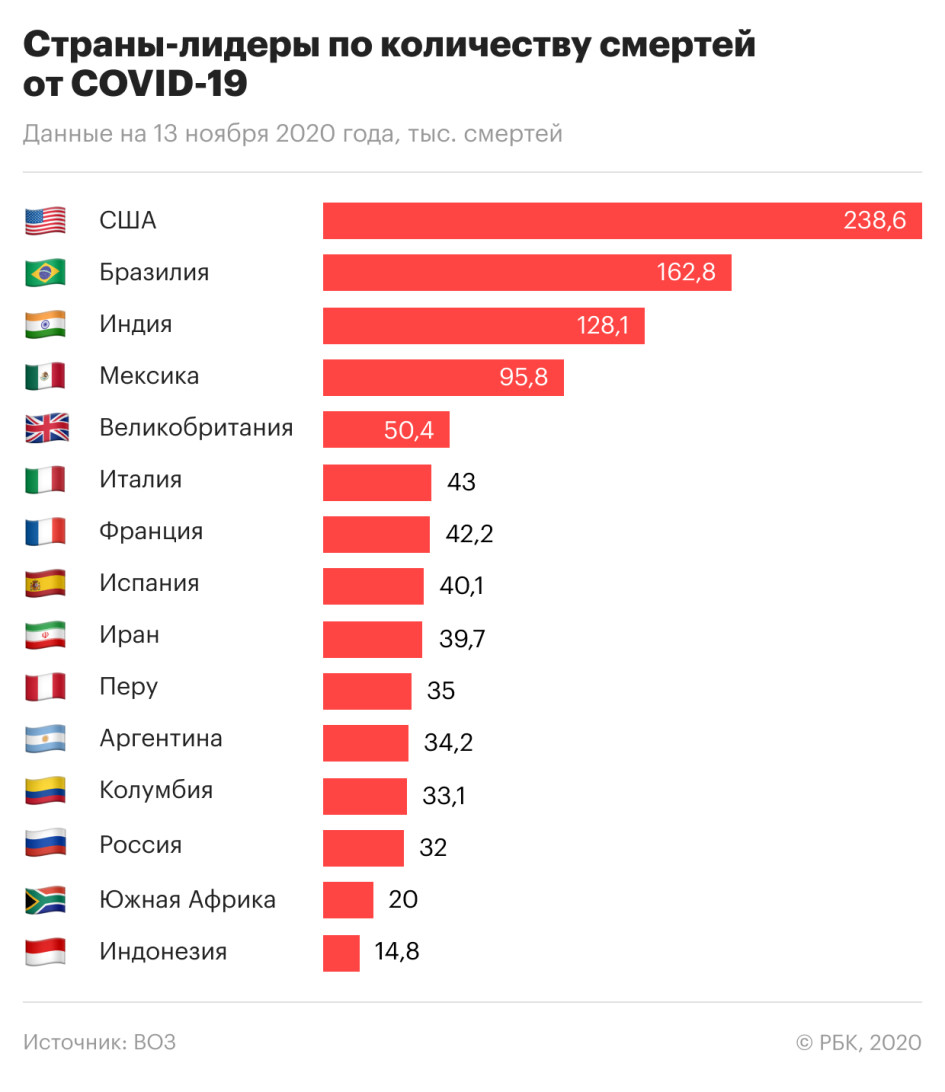
The countries most affected by COVID-19 in terms of the total number of deaths were the United States, Brazil and India. Italy, Spain and France – the European countries that were among the first to encounter the pandemic – are also stable in the top ten.
The list of countries with the most deaths per 1 million people looks similar, but the countries in it are distributed differently.
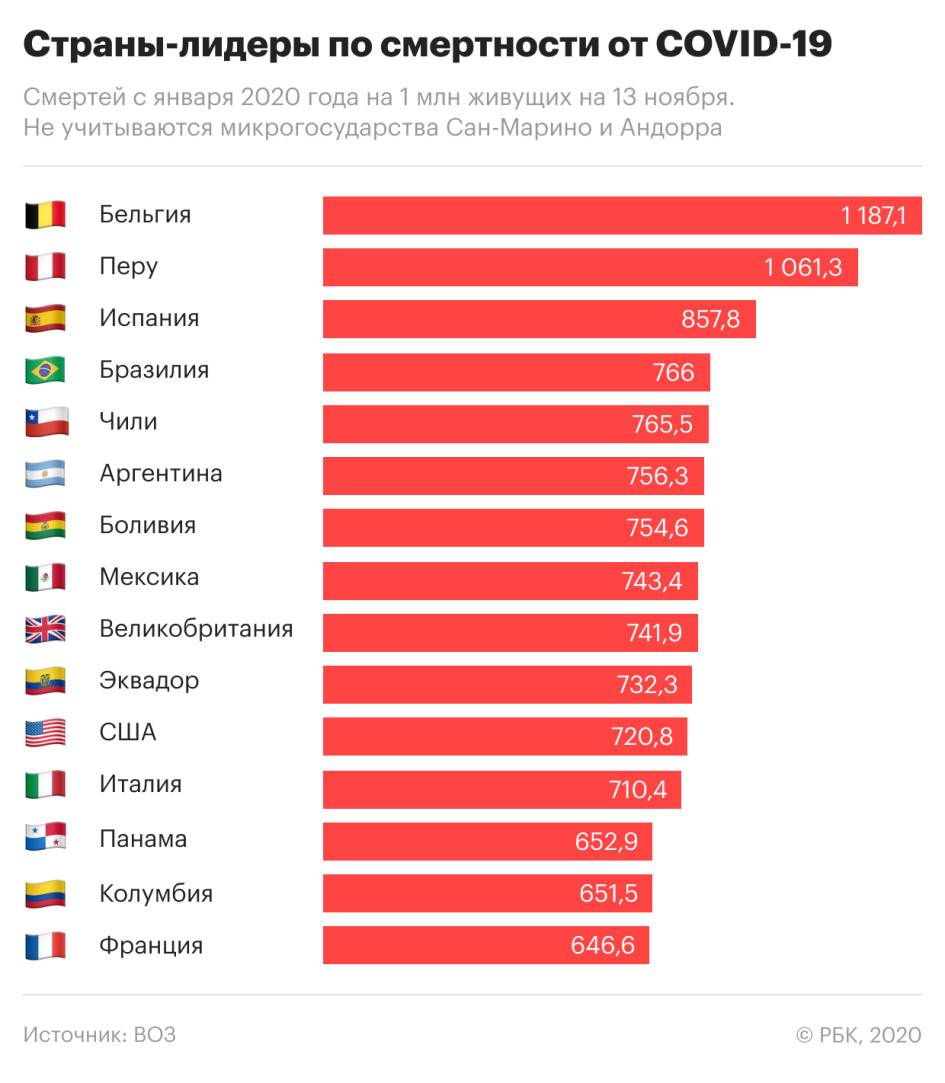
Russia, which is on the list of the top 15 countries in terms of the total number of deaths, ranks 54th (32,000 deaths) in calculating the number of COVID-19 victims per 1 million people. At the same time, it seems, the WHO is guided by the data of the operational headquarters for the fight against the coronavirus. At the same time, Rosstat shows many more deaths, relying on death certificates from the registry office: according to the latest data provided, from April to September, more than 55,000 Russians died with COVID-19.
What quarantine measures were returned to the Russian regions. the same thing

Influenza and COVID-19 have different age risk groups. In the first case, according to the WHO, the disease poses a danger to children, pregnant women and the elderly. As for the coronavirus, the elderly are mainly at risk here (and people of any age with chronic diseases, the same goes for the flu. RBK).
COVID Vaccine Creator predicts a harsh winter and a return to normal

In the article Age-specific mortality and immune patterns of SARS-CoV-2, published in the journal Nature in November, researchers collected confirmed data on the age distribution of deaths in 45 countries. RBC selected from this study 14 countries in Europe and Latin America with a total population of 627 million people and calculated the percentage of deaths in each age category (the sample is based on the comparability of the age groups considered in the study for these countries). COVID-19 has been found to be the most dangerous for seniors over the age of 70. This segment accounts for nearly two-thirds of all deaths.
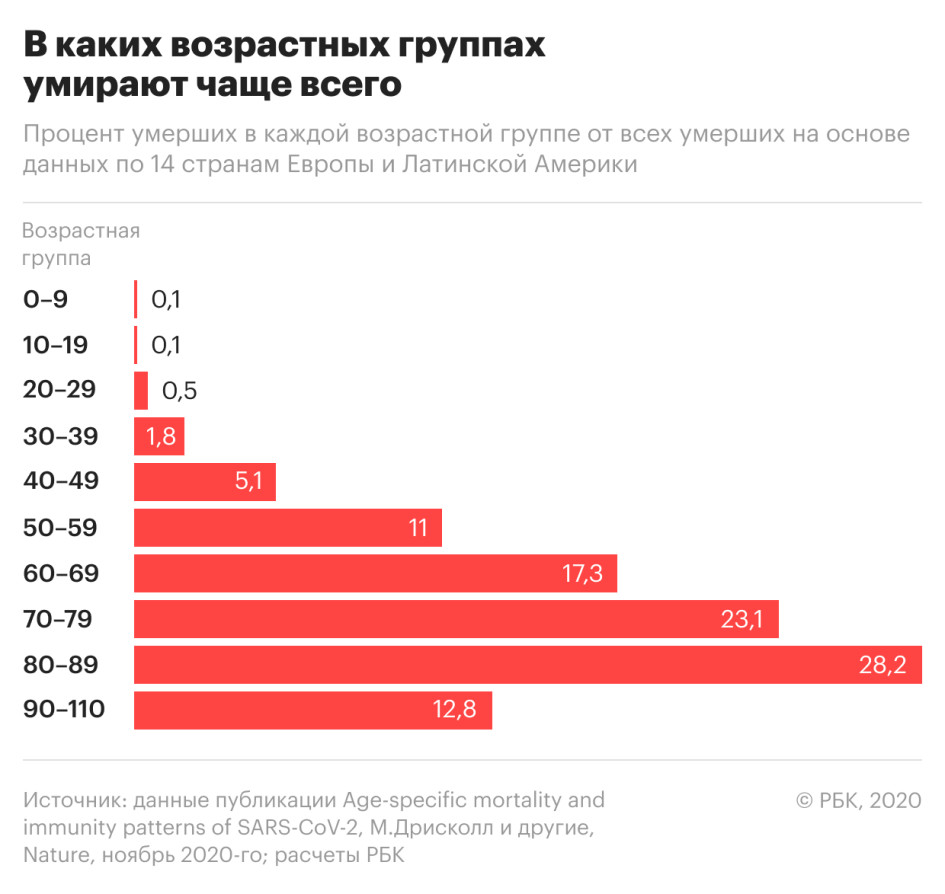
The disease is more easily tolerated by children. The 20-40 age group accounts for 2% of deaths. But people in these age groups who carry a mild infection can contribute to the spread of the disease.
Despite the fact that more age categories are attributed to influenza risk groups, with COVID-19 there are more cases of the disease in severe form, scientists say. This is because, in the case of flu, exposure to previous seasonal infections and mass vaccinations can limit the number of infections. But all people are potentially susceptible to the virus that causes COVID-19 due to its novelty.
When and for how long the patient is contagious
Another insidious feature of the coronavirus is the incubation period. The time from the time of infection to the onset of symptoms with COVID-19 averages five to six days, but can be up to 14 days. With the flu, the incubation period lasts on average two days, but it can be four. That is, with COVID-19, a person can potentially not feel the disease for longer.
The Ministry of Health explains the doctors’ infection with COVID after being vaccinated with the Gamalea vaccine

Recent studies also indicate that COVID-19 carriers remain infectious for longer. According to Rospotrebnadzor, with the flu, the patient becomes one day before the onset of the clinical manifestations of the disease. The maximum period in which a patient is contagious is three days of illness.
According to the WHO, people infected with the new type of coronavirus are most contagious two days before symptoms appear and at an early stage of the disease. Those who develop severe disease can spread COVID-19 for longer.
The U.S. Centers for Disease Control and Prevention (CDC) indicates that mild to moderate COVID-19 patients are contagious within ten days and immunocompromised patients for up to 20 days after symptoms appear.
Containment measures and use of masks
To curb the spread of the coronavirus, WHO recommends using a number of measures: in addition to wearing a mask, these include keeping distance, as well as frequent hand washing and disinfection. The effectiveness of the widespread use of masks has not been proven, but experts emphasize the need for their use in crowded places, for example, in public transport and shops (such requirements were introduced by Rospotrebnadzor throughout Russia since 28 October ).
Mishustin has criticized the regions for inappropriate actions on COVID-19

Demonstrations took place in Europe against measures taken by states, including the obligation to use personal protective equipment. And in Russia a petition against the compulsory use of masks appeared (by 15 November it was signed by just over 13 thousand people). The appeal, among other things, indicates the risks of self-infection due to improper or too long use of the mask (the WHO also indicates that masks must be used with care). And also that the mask can be useful precisely in terms of “reducing the potential risk of infection in contact with a patient during the period of the disease that precedes the onset of symptoms”. This is what the WHO draws attention to in its recommendations: “The mask can play the role of a barrier that holds back the spread of virus-infected respiratory droplets from an infected person.”
According to Rospotrebnadzor, wearing masks reduces the likelihood of contracting all types of respiratory infections by 1.8 times and wearing gloves by 1.3 times.
In one of the latest studies, Japanese scientists came to the conclusion that a cloth mask retains 17% of viral particles, a three-layer surgical mask – 47%, and an N95-type mask protects by 79%.
.
[ad_2]
Source link