
[ad_1]
“Pain”, sculpture by Jean Escoula (Musée d’Orsay) – © Fotios Stefanidis / Pexels 2020
- According to a study published by our partner The Conversation, more than 70% of French people suffering from chronic pain do not receive adequate treatment.
- Medical cannabis, which could alleviate them, will soon be the subject of an experiment conducted by the National Agency for the Safety of Medicines and Health Products (ANSM).
- The analysis of this phenomenon was carried out by Nicolas Authier, psychiatrist and pharmacologist at the CHU Clermont-Ferrand.
At least 12 million French people suffer from chronic pain, or permanent pain, suffered for at least three consecutive months, with significant physical, moral and social consequences.
In such conditions, pain becomes a disease in its own right, which has a lasting impact on the quality of life of patients. And this, especially since pain treatments are often insufficiently effective in the latter: in France it is estimated that over 70% of patients with chronic pain do not receive adequate treatment. This pathology leads to a high consumption of treatments and a significant professional absenteeism. It is therefore also an important economic and social issue.
In this context, medical cannabis enriches the range of therapeutic products available, while being part of the overall support of the patient with pain. Indeed, in countries that have legalized access to medical cannabis, chronic pain relief is the first indication for these products manufactured to pharmaceutical standards.
Cannabis and pain: how does it work?
Humans have a so-called “endocannabinoid” system, which plays an important role in the regulation of life processes (homeostasis). Composed of a set of receptors and endogenous substances (ie synthesized by the organism itself) that bind to it, this signaling system is very old in the animal kingdom. It has been well preserved throughout evolution, as it is found in all vertebrates.
The characterization of this neurotransmission system during the 1970s and 1980s initiated research into the value of its modulation in diseases such as chronic pain.
Different molecules produced by the plant Cannabis sativa L they have an action on the human endocannabinoid system. This is particularly the case with delta-9-tetrahydrocannabinol (more commonly known as THC), which can activate cannabinoid receptors CB1 and CB2 as well as other proteins involved in the transmission of pain messages to the brain.
 Cannabis leaves © Erin Stone / Pixabay
Cannabis leaves © Erin Stone / Pixabay
Cannabidiol (CBD), the other molecule found in cannabis, is said to have less affinity for cannabinoid receptors. However, it modulates the effect of THC on its receptors and limits its unwanted effects, especially neuropsychiatric (sleepiness, anxiety, etc.). CBD also enhances system activation by inhibiting the breakdown of an endocannabinoid, anandamide. Its activating action on the serotonin receptors would explain its anxiolytic effect. Finally, CBD would bind to many other receptors involved in inflammation and pain perception.
The beginning of scientific validation
The evaluation of the benefit of medical cannabis in a large number of painful clinical situations has been the subject of scientific publications, however the levels of evidence often remain modest, even low, during conventional clinical trials comparing it to a placebo.
Many clinical trials have focused on the use of medical cannabis to treat musculoskeletal pain, especially spasticity, a painful muscle contraction. This disorder would affect not only up to 25% of the 100,000 French people with multiple sclerosis, but also those with a spinal cord injury or sequelae following a stroke. Sativex, a drug based on cannabis extract, obtained marketing authorization in 2014 for this indication but is not yet marketed, due to the lack of agreement on the selling price between the authorities and the laboratory. who markets it.
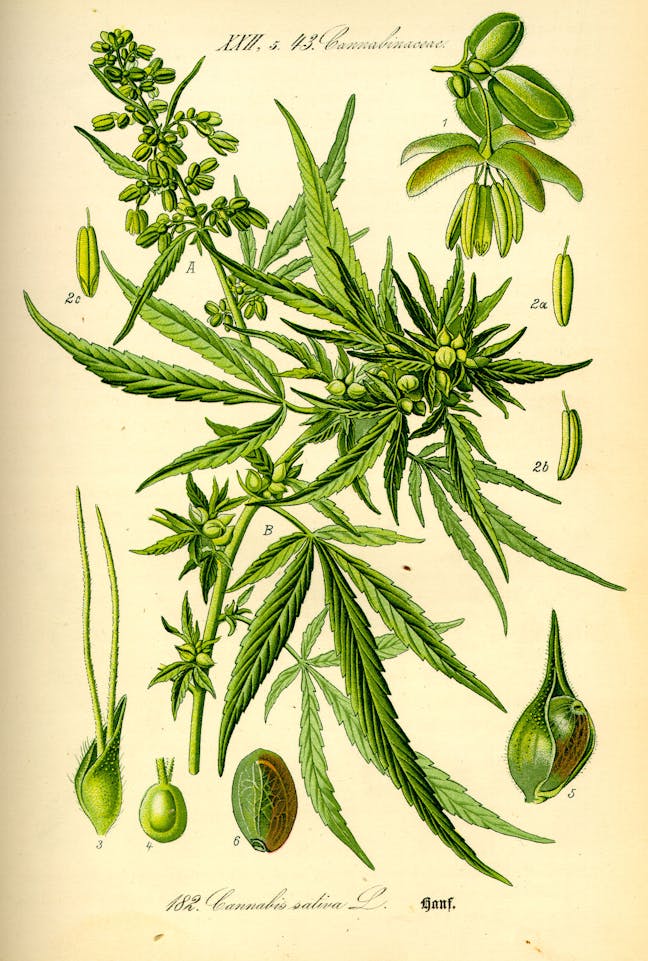 Cannabis sativa L. © Wikimedia – Kurt Stueber, CC BY SA 4.0
Cannabis sativa L. © Wikimedia – Kurt Stueber, CC BY SA 4.0
The health benefit of cannabis products has also been shown in neuropathic pain. This type of pain, which affects 7% of French people (i.e. a quarter of people suffering from chronic pain), results from an injury or disease of the somatosensory system. It comes in the form of a series of painful symptoms (intense tingling, electric shock, crushing sensation, burning or stabbing, etc.) for which the recommended drug treatments, antidepressants or antiepileptics, are only partially. effective and sometimes poorly tolerated.
These two conditions are the main indications of chronic pain withheld in the French experiment that will be piloted by the National Agency for the Safety of Medicines and Health Products (ANSM), from 2021 to 2023: 1,500 of the 3,000 people who will be treated during will be affected experimentation.
French patients prone to very frequent pain will also experiment with medical cannabis. This is especially true for those suffering from palliative care indications (500 patients to be recruited) and cancer-related complications (500 patients to be recruited).
Other chronic pain is the subject of research work all over the world, with sometimes encouraging results, but which have yet to be scientifically confirmed by methodologically more rigorous studies.
This is the case with the therapeutic use of cannabis in fibromyalgia, some chronic headaches, endometriosis, sickle cell anemia or bone and joint pain.
Neither the alpha nor the omega of pain treatment
Cannabis-based drugs are by no means the promise of a pain-free life; they must be part of the overall pain patient care. The therapeutic goal of their use to treat chronic pain goes beyond simply relieving pain intensity, although this is often considered the primary goal in clinical trials.
Medical cannabis could also have a positive impact on pain-related ailments such as mental distress or sleep disturbances. The ultimate goal is to improve the quality of life of a patient suffering from a chronic disease, to allow him to no longer devote his vital energies to the fight against this pain. It is also to help him work better on accepting this “pain disease” and to find more regular physical activity, as well as more positive thoughts.
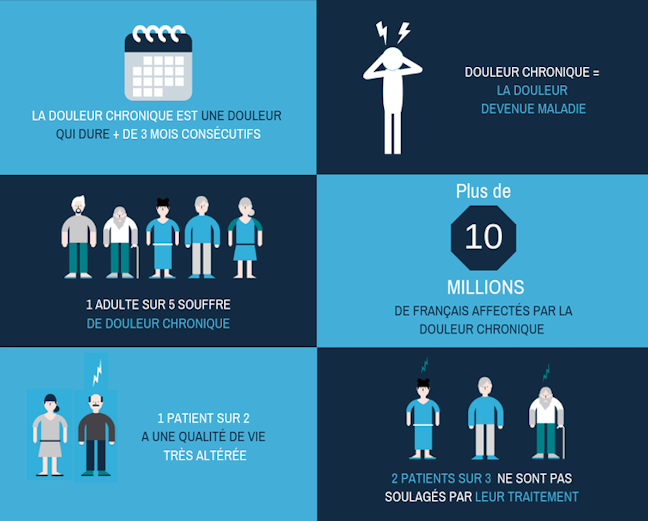 Chronic pain affects several million people in France © Analgesia Foundation, N. Authier
Chronic pain affects several million people in France © Analgesia Foundation, N. Authier
The French experiment will provide the opportunity to determine the potential placement of these drugs and their prescription methods in proposed therapeutic strategies to counter chronic pain. With this in mind, the choice of products based on their composition, particularly in THC and CBD, and the adjustment of dosages still need to be clarified.
Go towards personalized medicine
Treating a patient with chronic pain shouldn’t be centered around prescribing drugs, which are only part of the solution. On the contrary, research on medical cannabis and pain must be part of precision medicine.
It must aim at relevant therapeutic goals, focused more on the painful patient than on the mere disappearance of his pain.
For this, complementary approaches that combine real-life studies and conventional clinical trials against placebo or reference drugs must be implemented.
In addition, the entourage effect should be better studied, according to which the combination of several compounds contained in the plant would be more effective than if the cannabinoids (THC, CBD, etc.) were administered alone. It is often invoked to justify the administration of the totum of the plant (whole plant or part of a plant used as it is, and therefore containing many molecules). Cannabis-based drugs are therefore complex mixtures of several dozen or even hundreds of substances. The possible part of other cannabinoids and some terpenes in their effectiveness will have to be evaluated, to optimize the final composition.
Ultimately, it will be a question of determining more precisely which cannabis product can be prescribed to which patient in order to have the maximum chance of achieving the therapeutic goal. This will improve the cost effectiveness of these drugs and avoid too risky, or even too many prescriptions, as we sometimes see in painful patients who are undergoing excessive but not relieved medications.
This analysis was written by Nicolas Authier, psychiatrist and pharmacologist at CHU Clermont-Ferrand, professor of medicine at the University of Clermont-Auvergne. The original article was posted on the website of The conversation.

Source link