[ad_1]
“Lung metastases deplete certain types of chemokines from their local environment, which means that the signal that should attract beneficial white blood cells to fight cancer is gone. We hypothesized that delivering that chemokine signal to the tumor site could help restore the body’s normal immune response and allow it to attack tumors, “said co-first author Anvay Ukidve, a former graduate researcher at the Wyss Institute and SEAS who he is now a scientist at a pharmaceutical company.
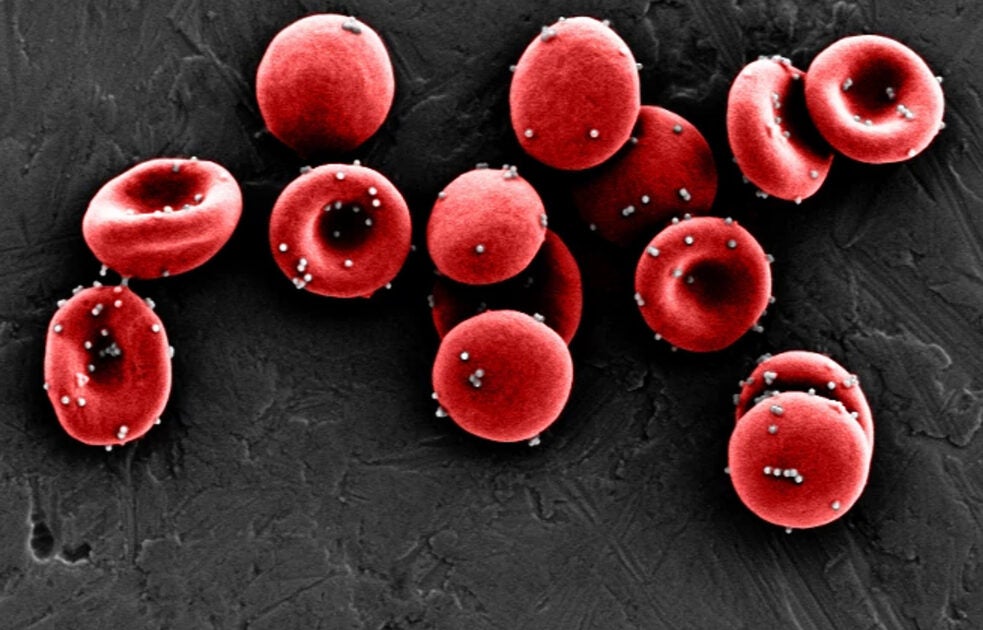
The team first optimized their nanoparticles to ensure that they only detach from their red blood cell hosts when the blood cells made their squeeze through the tiny capillaries of the lungs. They also decorated the surfaces of the nanoparticles with an antibody that binds to a protein commonly found on lung blood vessel cells called ICAM-1 to increase retention of the nanoparticles in the lungs. These nanoparticles were then filled with CXCL10 chemokine, creating a package that the researchers called ImmunoBait. The ImmunoBait particles were then attached to the mice’s red blood cells to create a therapeutic delivery system called systemic red cell-anchored immunotherapy (EASI) and injected into the bloodstream of mice with breast cancer that had metastasized to the lungs.
The ImmunoBait particles remained in the lungs of the animals for up to six hours after the EASI injection and most of them were distributed in and around the metastases. Treatment with EASI resulted in strong expression of CXCL10 for up to 72 hours, suggesting that administration of the chemokine stimulated the body to start producing it on its own, despite the immunosuppressive tumor microenvironment. To find out exactly what effect the delivered CXCL10 had on the mice’s immune systems, the team analyzed the different cell types present in the lungs before and after the EASI injection. They observed increases in the infiltration of CD4 T helper type 1 (Th1) cells, which release pro-inflammatory chemicals that help keep tumors in check, as well as effector CD8 cells and natural killer (NK) cells, which guide the direct killing of cancer cells.
Inject locally, protect globally
Armed with evidence that their system could attract immune cells to lung metastases, the team then tested its ability to slow or stop disease progression in mice. They first removed the animals’ breast cancer tumors (to mimic the surgery patients often undergo to treat their primary tumors), then injected them with just CXCL10, ImmunoBait nanoparticles alone, or EASI.
EASI inhibited the progression of lung metastases with four-fold and six-fold efficacy compared to free CXCL10 and ImmunoBait, respectively. All EASI-treated mice had fewer than 20 metastatic nodules after 37 days, and 25% of them had only one nodule. In contrast, the mice that received the other therapies had two to 100 nodules. The mice that received EASI also had nearly three times better survival: while animals in all other treatment groups died from their disease in less than 20 days, about 25% of mice treated with the EASI survived for 40 days. They were also free of any signs of off-target toxicity or other adverse effects of treatment.
Because EASI effectively activated the immune system against lung metastases, researchers wondered whether that activation could provide lasting protection against future relapses of the same cancer. They analyzed the blood of mice that had received EASI and observed an increase in the number of memory CD8 cells, which persist long-term after an immune threat and can raise the alarm if that threat recurs. To test whether those memory cells provided sufficient protection, the team re-inoculated the mice with the same cancer cells two days after their last treatment. Mice that were treated with EASI had significantly lower tumor growth and tumor weight than mice that were injected with saline or untreated, demonstrating that local treatment of lung metastases produced systemic immunity against development of the tumor.
“These results highlight the ability of our EASI system to convert the biological adversities of metastases into a unique therapeutic opportunity against metastatic cancers,” said senior author Mitragotri, who is also Hiller Professor of Bioengineering and Hansjörg Wyss Professor of Biologically. Inspired Engineering at SEAS. His team is continuing to optimize EASI by experimenting with the delivery of different types of chemokines via ImmunoBait nanoparticles and exploring the combination of EASI with currently approved cancer therapies to identify potential synergies.
“This unique bio-inspired approach to cancer therapy is a wonderful example of the outside-the-box thinking we encourage and support at the Wyss Institute, harnessing the body’s red blood cells to deliver drugs to the capillary blood vessels in the lung where many metastases form, the team of Samir has developed a completely new type of immunotherapy and has opened the door to potentially life-saving therapies, “said the founding director of the Wyss Institute. Don Ingber who is also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the Vascular Biology Program at Boston Children’s Hospital, as well as a professor of bioengineering at SEAS.
Other authors of the article are current Wyss and SEAS members Yongsheng Gao and Jayoung Kim; former Wyss and SEAS members Vinu Krishnan, Daniel Pan, Michael Evans and Abhirup Mandal; former SEAS student Alexandra Fehnel; Junling Guo, former colleague of the Wyss Institute; and Vladimir Muzykantov of the University of Pennsylvania’s Perelman School of Medicine.
This research was supported by the Wyss Institute for Biologically Inspired Engineering and the National Institutes of Health.
Source link