[ad_1]
As the pandemic continues to hit many countries head-on, doctors are still working to better understand the impact of the coronavirus on the body, and in particular its medium and long-term impact; effects described as part of the “long COVID”. Several studies have shed light on neurological symptoms and abnormalities found in patients who contracted the virus, and recently, a team of researchers compiled records of 70 million patients to show that nearly 18% of them had the disorders. psychiatric patients within three months of infection.
According to one study, nearly one in five people who have contracted COVID-19 are diagnosed with a psychiatric disorder such as anxiety, depression, insomnia, or even dementia within three months of testing positive for the virus. suggests that action is needed to ease the mental health toll caused by the pandemic.
The analysis, conducted by researchers at the University of Oxford and the NIHR Oxford Health Biomedical Research Center, also found that people diagnosed with a pre-existing mental disorder were 65% more likely to be diagnosed with COVID-19 than to those who have not, even taking into account known risk factors such as age, sex, ethnicity and underlying physical condition.
Psychiatric disorders diagnosed in 18% of patients
” This discovery was unexpected and requires investigation. In the meantime, having a psychiatric disorder should be added to the list of risk factors for COVID-19 Says Max Taquet, a researcher at NIHR. The calculations were made on the basis of approximately 70 million US medical records, including more than 62,000 cases of Covid-19 that required no hospitalization or emergency room visits.
The incidence of a psychiatric disorder diagnosis within 14-90 days of Covid-19 diagnosis was 18.1%, of which 5.8% was a first diagnosis. To examine whether the excess risk was directly associated with Covid-19, the researchers compared the data with six other diseases during the same period: influenza; other respiratory tract infections; skin infection; gallstones; urinary tract stones; and a big broken bone.
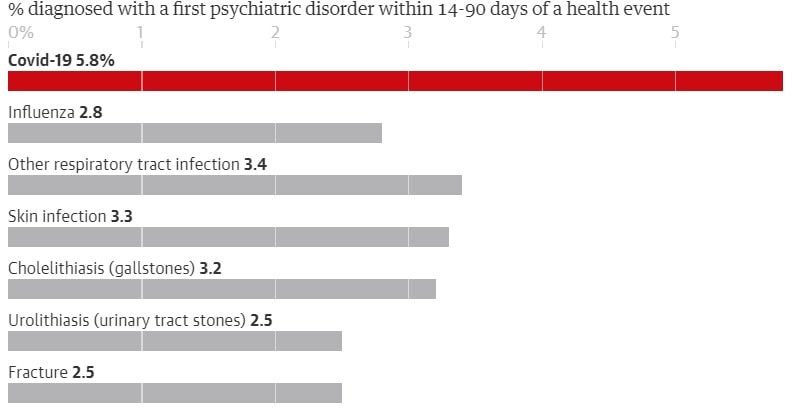
Within three months of Covid-19 diagnosis, 5.8% of patients had the first recorded diagnosis of psychiatric illness, compared with 2.5% -3.4% of patients in the comparator cohorts – nearly a doubling in risk , according to the article published in the journal The Lancet Psychiatry.
Further research to interpret these results
Paul Harrison, a professor of psychiatry at the University of Oxford, explains that more research is needed to determine whether a diagnosis of psychiatric disorder could be directly linked to a coronavirus infection. General factors affecting physical health were not taken into account in the files analyzed, such as socioeconomic history, smoking or drug use. It is also possible that the general stressful environment of the pandemic is playing a role.
Research suggests that people from poorer socioeconomic backgrounds are more likely to suffer from mental health problems. Poverty also increases exposure to the coronavirus, due to factors such as overcrowded housing and unsafe working conditions. ” Likewise, it’s not at all unlikely that COVID-19 could have a direct effect on the brain and mental health. But I think, again, this needs to be explicitly demonstrated Harrison says.
Of particular interest was the doubling of the diagnosis of dementia – which is usually irreversible – three months after the positive result for Covid-19, compared to other health problems. Going to the hospital or seeing your doctor to get a diagnosis of Covid-19 can help diagnose other pre-existing conditions, such as dementia, according to Harrison.
Get a better understanding of the effects of the coronavirus on the brain
” That said, it is by no means unlikely that there could be a brain effect of the virus in some people as well, which would cause some additional neurological symptoms and difficulties. We are therefore particularly careful not to over-interpret this association. Harrison adds.
Studies on the impact of the virus on the brain and central nervous system are underway, including one from British scientists who have formed a partnership to explore the neurological and neuropsychiatric complications of Covid-19. In July, neurologists released details of over 40 UK patients whose complications ranged from brain inflammation and delirium to nerve damage and stroke.
Only time will tell whether the incidence of psychiatric illness after Covid-19 will continue to increase or persist beyond the three-month period. ” It is difficult to judge the importance of these findings … perhaps unsurprisingly it happens a little more often in people with Covid-19, who rightfully feared becoming seriously ill and who will also have had to endure a period of isolation. »Concludes David Curtis, a professor at University College London.
Sources: The Lancet Psychiatry
Source link