
[ad_1]
It is particularly difficult to estimate the magnitude and severity of the Covid-19 pandemic that has shaken the planet since the beginning of the year, because the data collected is very heterogeneous. Often used as an indicator, the number of deaths is representative of only a small percentage of infections. In addition, the data available vary by country, especially with regard to deaths of the elderly.
Based on mortality data by age group as well as the results of 22 seroprevalence studies, i.e. the search, in blood samples, for antibodies directed against SARS-CoV-2 (which testifies to an infection with this coronavirus), the Researchers at the University of Cambridge and the Pasteur Institute have estimated, in 45 countries, the percentage of the population that has been infected with 1is September 2020.
Overall, this analysis confirms that vaccine-free herd immunity remains a very difficult target. In other words, while waiting for the vaccine, we have no choice but to continue to wear the mask, keep a distance from each other in public places, ventilate closed places and respect the measures. hygiene if we want to slow the progression of the coronavirus. Here’s what we learn from this work.
Refined comparisons of the incidence of Covid-19 between countries
To assess the dynamics and severity of an epidemic, various indicators are available: the number of cases of infections, the number of deaths, the baseline reproduction rate (average number of people infected with a person infected with the virus), the doubling time of cases (time required to double the number of infected people), hospital occupancy rate, etc.
This multiplicity of indicators means that comparing situations between different countries can be a dangerous exercise, for several reasons. First of all, the profiles of the populations (age, sex, comorbidities, etc.) are heterogeneous. Second, not all countries are the same when it comes to testing and surveillance capabilities, which can make it difficult to estimate the number of cases. Finally, the definition of what constitutes a case of infection can also vary from one country to another, depending, for example, on whether it is based on the performance of a single RT-PCR test or two subsequent examinations, which are taken in consideration for clinical symptoms via a chest X-ray, etc.
As a result, mortality data based on death certificates are often considered a more reliable indicator, although the attribution of causes of death may also vary from country to country. Based on these data, the authors of this work demonstrated that they can be used in conjunction with the mortality rate from infection (Relationship between infections and fatality or IFR in English, in other words the ratio of the number of deaths to the number of infected people) to estimate the total number of SARS-CoV-2 infections This number is greater than the number of cases detected, which depends on the test.
By matching these data with the results of seroprevalence surveys, the authors were also able to estimate IFRs by age and by location. This is important because simply comparing mortality between countries without taking into account the age structure of the population can provide a misleading representation of the level of transmission of SARS-CoV-2.
More reliable mortality data among the under 65s
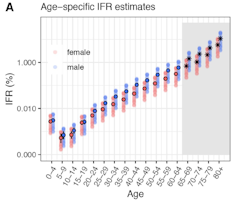
O’Driscoll M. et al (2020)
The authors of this work found that the lowest mortality was in children aged 5-9 (IFR of 0.001%). For people aged 30 to 65, the relative risk of death increased with age in a log-linear relationship (which follows a Poisson regression model). Over the age of 65, the risk of mortality was much more variable, albeit increasing (in people aged 80 and over the IFR averages 8.29% for both genders.).
It should be noted, however, that data for people over 65 may be less reliable and mortality figures underestimated due to the problem of reporting deaths in nursing homes and retirement homes. Therefore, in the UK, Canada and Sweden, Covid-19 still significantly infected nursing home residents with 20% deaths. In fact, once the virus has entered a nursing home, it can rapidly spread within a fragile population. Conversely, some countries in Asia and South America have reported significantly fewer deaths from Covid-19 among the elderly than expected. The authors believe that in some countries this reflects the success of elder protection policies, while in other countries (Ecuador, for example) these figures could be linked to errors.
This work also demonstrated a significantly higher risk of death in men than in women, especially in people of advanced age: in the 80s and over the IFR for men is 10.8% while that of women is 5.6%. .
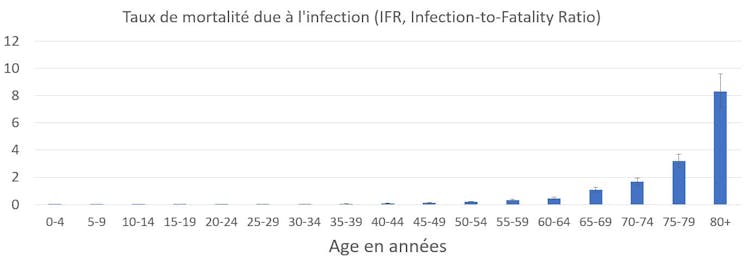
O’Driscoll M. et coll. (2020)
Only a small fraction of the populations have antibodies
This IFR enabled the researchers to develop a mathematical model to estimate what fraction of the population would likely develop antibodies to the SARS-CoV-2 coronavirus, taking into account age, gender, sensitivity and specificity of 1-point tests.is September 2020.
The results obtained vary from 0.06% in South Korea to 62.44% in Peru. Global modeling shows that Latin American countries have been heavily affected by the outbreak: estimated seroconversion is particularly important in Peru (62.44%), Mexico (45.6%) and Ecuador (44.7%). However, the uncertainty levels of estimates are high for these countries, reflecting the uncertainties of subnational surveys on individual seroprevalence.
Conversely, South Asian countries appear to have suffered far fewer infections. This is the case, for example, of Japan (0.1%), China (0.09%) and Thailand (0.08%). Another study published in the Bulletin of the World Health Organization obtained similar estimates of seroprevalence: these ranged from 0.02% in Shijiazhuang, China, to 58.4% in Indian slums.
It should be noted here that there are still many questions about the duration and form of the immune response (antibody and lymphocyte response) to infection with this coronavirus, and that the presence of antibodies is not necessarily synonymous with neutralizing SARS-CoV-2nbsp; . Neutralizing antibodies must be directed specifically against its spike protein S, which acts as a “key” to enter cells.
For this reason, although several recent studies have recently suggested that some antibodies against SARS-CoV-2 may persist for up to 5 months in the body (with a decline over time), we must remain cautious about their interpretation.
Furthermore, the immune response has mainly been studied in hospitalized patients; knowledge is much lower for asymptomatic cases. In addition, some rare cases of reinfection in young patients have been reported in the literature in Belgium, the United States, Ecuador or Hong Kong.
The situation in France
In our country, the authors estimate that an average of 3.38% to 4.63% of the general population has anti-SARS-CoV-2 antibodies. In nursing homes, 7.28% of the population would be infected, which is explained by the fact that the attack rate (the rate of accumulation of new cases) was 1.7 times higher than in the general population.
These results are consistent with data from the EpiCoV survey, based on serological analyzes of 12,000 participants. These show that in May-June the seroprevalence was 4.5% in France. The Upper Rhine and Paris had the highest percentages of people testing positive (10.8% and 9%, respectively), while the lowest percentages were found in Occitania or Normandy (1.9%).
Another survey, SAPRIS, focused on three cohorts in the general population (Constances, E3N-E4N, NutriNet-Santé, and Elfe-Epipage2), with a total of 14,600 serological results. According to the results, the percentage of inhabitants of the Grand-Est, Île-de-France and Nouvelle-Aquitaine regions possessing anti-SARS-CoV-2 antibodies is 9%, 10% and 3.1% respectively (which is consistent , the Nouvelle-Aquitaine region was less affected by the first wave).
The limits of these mortality data and seroprevalence surveys
The use of such data by country has some limitations. We know in particular that there is considerable variation within a country in terms of transmission of the infection, as the situations of the various French regions during the first wave showed.
There may also be people who never seroconvert, or who only develop a response involving T cells and who will be “lost” by serological testing. Additionally, some asymptomatic cases may have their antibody level rapidly decreasing over time.
Another limiting point concerns the attribution of causes of death. It can be difficult to distinguish patients who have died as a direct consequence of infection with the SARS-CoV-2 coronavirus and associated deaths, for example due to lack of access to medical interventions or treatment (in the case of asthma or diabetic patients for example).
An undiagnosed Covid-19 can also lead to exacerbation of a pre-existing disease, which can lead to premature death. Delays in the diagnosis and treatment of various types of cancer, for example, can allow the cancer to progress and affect patient survival. Another example: Fear of exposure to the virus has prevented many patients with heart problems from going to hospital, putting them at a greater risk of long-term complications of myocardial infarction.
To account for these indirect cases, excess mortality – excess deaths over normal – is a good indicator. It is calculated by comparing the weekly deaths in the current year with an “expected value” based on the average of the previous five years. In this way, it is possible to understand the indirect mortality due to Covid-19.
Finally, the last limiting point in the use of mortality and seroprevalence data: in some countries where the tests have failed and whose surveillance system is not sufficiently developed, it can be difficult to get a precise idea of the situation. The authors of the work published in the journal Nature to report, for example, that it was estimated that, for 6 of the countries included in their analysis, deaths due to Covid-19 could have been underestimated (up to 40%) or overestimated (up to 10%). For this reason, some experts believe that when the health system has outgrown its capabilities, all deaths can be attributed, in one way or another, to the pandemic.
However, despite these uncertainties about the number of deaths, this work demonstrates that reliable estimates can be obtained from global seroprevalence data. This approach can be useful for countries or regions that do not have the means to set up an HIV prevalence survey.
Source link