[ad_1]
/ 7activestudio, stock.adobe.com
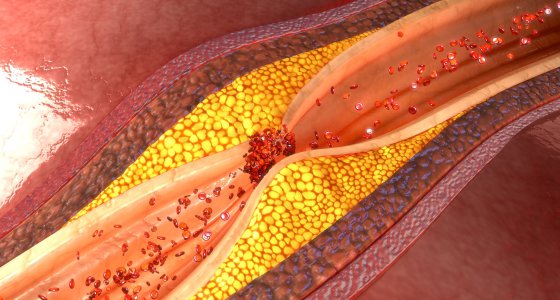
Ann Arbor, Michigan – Blood clots in small blood vessels that often contribute to the catastrophic course of COVID-19 may be due to the same autoantibodies that lead to thrombotic complications in antiphospholipid syndrome, according to rheumatologists’ observations.
The publication in Scientific translational medicine (2020; DOI: 10.1126 / science.abd3876) could have an impact on treatment strategies.
It was noted early in the pandemic that many COVID-19 patients had an increase in D-dimers. This was initially interpreted as a sign of dissiminated intravascular coagulation, but the concentration of the clotting factors that are consumed in this disorder is not reduced in COVID-19 patients.
It is more likely to lead to thrombotic disorders, which have been seen in autopsies, especially in the smaller blood vessels. There is a parallel here with antiphospholipid syndrome, which is also associated with an increased tendency to thrombosis.
Antiphospholipid syndrome is triggered by various autoantibodies to phospholipids and phospholipid-binding proteins, which include prothrombin and beta-2-glycoprotein I.
A team led by Yogen Kanthi of the University of Michigan at Ann Arbor has now detected these antibodies in 89 of 172 patients (52%) hospitalized for severe COVID-19. In 52 patients (30%) the antibody titer was significantly increased. Detection of antibodies has been associated with a more severe course of the disease and especially with kidney damage.
An association was found with an increase in serum calprotectin (a marker for neutrophil activation) and with an increase in myeloperoxidase-DNA complexes, indicating “neutrophil extracellular traps” (NETs).
NETs are a primitive defense reaction of the immune system in which neutrophil granulocytes “explode” to trap pathogens with the resulting DNA released, like in a trap. NET is also believed to be involved in the pathogenesis of antiphospholipid syndrome. The autoantibodies are supposed to cause the immune cells to “explode”.
As early as April, researchers were able to show that there is also an increase in NET release in COVID-19. Their current study suggests that the aPL antibodies that have now been detected may be responsible.
This is supported by laboratory tests in which IgG antibodies from the blood of COVID-19 patients resulted in the release of NETs by neutrophil granulocytes of healthy volunteers. On the other hand, the researchers were able to trigger thrombosis in mice by injecting IgG antibodies from COVID-19 patients.
The findings shed new light on the pathogenesis of COVID-19 and may question current treatment attempts. In serum therapy, patients receive plasma from people who have survived COVID-19. The convalescent’s blood antibodies should intercept the viruses.
However, if the donor serum also contains antiphospholipid antibodies, this could increase the patient’s tendency to thrombosis. This would explain why serum therapy has not so far shown clearly positive results in studies.
Another consequence of the current findings would be that therapies developed for antiphospholipid syndrome could also be effective for COVID-19. In addition to treatment with heparins (which are now used in COVID-19 patients), this includes treatment with the antithrombotic dipyridamole.
US doctors were able to show in a previous study that dipyridamole inhibits the release of NETs. In a Phase 2 study, they are now looking into whether dipyridamole can prevent COVID-19 from worsening in the clinic. © rme / aerzteblatt.de
.
[ad_2]
Source link