[ad_1]
Alzheimer’s disease is the most common cause of dementia. Still incurable, it directly affects nearly one million people in Europe and indirectly millions of family members and society as a whole.
In recent years, the scientific community has suspected that the gut microbiota plays a role in the development of the disease.
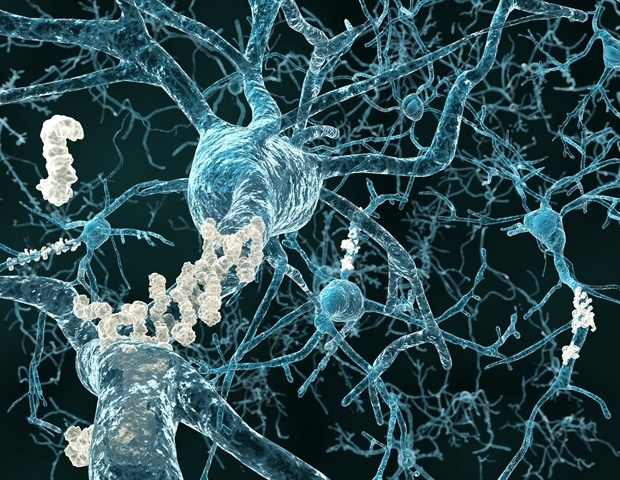
A team from the University of Geneva (UNIGE) and the University Hospitals of Geneva (HUG) in Switzerland, together with Italian colleagues from the National Center for Research and Treatment for Alzheimer’s and Psychiatric Diseases Fatebenefratelli of Brescia, University of Naples and IRCCS SDN Research Center in Naples, confirm the correlation, in humans, between an imbalance of the intestinal microbiota and the development of amyloid plaques in the brain, which are at the origin of the neurodegenerative disorders characteristic of Alzheimer’s disease.
The proteins produced by certain intestinal bacteria, identified in the blood of patients, could in fact modify the interaction between the immune system and the nervous system and trigger the disease.
These results, to be discovered in Journal of Alzheimer’s Disease, allow to foresee new preventive strategies based on the modulation of the microbiota of people at risk.
The research laboratory of neurologist Giovanni Frisoni, director of the HUG Memory Center and professor at the Department of Rehabilitation and Geriatrics of the UNIGE Faculty of Medicine, has been working for several years on the potential influence of the intestinal microbiota on the brain, and more particularly on diseases neurodegenerative.
“We have already shown that the composition of the gut microbiota in patients with Alzheimer’s disease was altered, compared to people who do not suffer from these disorders,” he explains. Their microbiota has in fact a reduced microbial diversity, with an overrepresentation of some bacteria and a strong decrease of other microbes.
Furthermore, we also found an association between an inflammatory phenomenon detected in the blood, some intestinal bacteria and Alzheimer’s disease; hence the hypothesis we wanted to test here: can inflammation in the blood be a mediator between the microbiota and the brain? “
The brain under influence
Gut bacteria can affect brain functioning and promote neurodegeneration through various pathways: they can influence the regulation of the immune system and, consequently, can modify the interaction between the immune system and the nervous system.
Lipopolysaccharides, a protein located on the membrane of bacteria with pro-inflammatory properties, have been found in the amyloid plaques and around the brain vessels of people with Alzheimer’s disease.
Furthermore, the intestinal microbiota produces metabolites – in particular some short-chain fatty acids – which, having neuroprotective and anti-inflammatory properties, directly or indirectly affect brain function.
To determine whether inflammatory mediators and bacterial metabolites make a link between the gut microbiota and amyloid pathology in Alzheimer’s disease, we studied a cohort of 89 people between 65 and 85 years of age.
Some suffered from Alzheimer’s or other neurodegenerative diseases that caused similar memory problems, while others had no memory problems ”, reports Moira Marizzoni, researcher at the Fatebenefratelli Center in Brescia and first author of this work.
Using PET imaging, we measured their amyloid deposition and then quantified the presence in the blood of various inflammation markers and proteins produced by gut bacteria, such as lipopolysaccharides and short-chain fatty acids. “
A very clear correlation
“Our results are indisputable: some bacterial products of the intestinal microbiota are correlated with the amount of amyloid plaques in the brain,” explains Moira Marizzoni.
Indeed, elevated blood levels of lipopolysaccharides and some short-chain fatty acids (acetate and valerate) were associated with both large amyloid deposits in the brain. Conversely, high levels of another short-chain fatty acid, butyrate, were associated with less amyloid pathology.
This work therefore provides evidence of an association between some intestinal microbiota proteins and cerebral amyloidosis through an inflammatory phenomenon of the blood. Scientists will now work to identify specific bacteria, or a group of bacteria, involved in this phenomenon.
A strategy based on prevention
This discovery paves the way for potentially highly innovative protective strategies – through the administration of a bacterial cocktail, for example, or pre-biotics to feed the & laquogood »bacteria in our gut.
However, we shouldn’t be too quick to rejoice, says Frisoni. In fact, we must first identify the varieties of the cocktail. Therefore, a neuroprotective effect could be effective only at a very early stage of the disease, from a prevention rather than a therapy perspective.
However, early diagnosis is still one of the main challenges in managing neurodegenerative diseases, as protocols must be developed to identify high-risk individuals and treat them well before detectable symptoms appear.
This study is also part of a larger prevention effort led by the UNIGE Faculty of Medicine and the HUG Memory Center.
Source:
Journal reference:
Moira, M., et al. (2020) Short-chain fatty acids and lipopolysaccharides as mediators between intestinal dysbiosis and amyloid pathology in Alzheimer’s disease. Journal of Alzheimer’s Disease. doi.org/10.3233/JAD-200306.
.
[ad_2]
Source link