[ad_1]
PROVIDENCE, RI [Brown University] – A new study on airflow patterns inside a car’s passenger compartment offers some suggestions for potentially reducing the risk of transmitting COVID-19 by sharing journeys with others.
The study, led by a team of researchers from Brown University, used computer models to simulate the flow of air inside a compact car with various combinations of open or closed windows. Simulations showed that opening windows – the more windows, the better – created airflow patterns that dramatically reduced the concentration of airborne particles exchanged between a driver and a single passenger. Researchers found that blowing up the car’s ventilation system didn’t circulate the air as well as some open windows.
“Driving around with the windows open and the air conditioning or heating on is definitely the worst case scenario, according to our computer simulations,” said Asimanshu Das, a graduate student at Brown’s School of Engineering and co-lead author of the Research. “The best scenario we found was having all four windows open, but even having one or two open was much better than having all of them closed.”
Das co-conducted the research with Varghese Mathai, a former postdoctoral researcher at Brown who is now an assistant professor of physics at the University of Massachusetts, Amherst. The study is published in the journal Science Advances.
Researchers point out that there is no way to completely eliminate the risk, and of course, current guidelines from the U.S. Centers for Disease Control (CDC) find that postponing travel and staying home is the best way to protect health. personal and community. The goal of the study was simply to investigate how changes in airflow inside a car can worsen or reduce the risk of pathogen transmission.
The computer models used in the study simulated a car, loosely based on a Toyota Prius, with two people inside: a driver and a passenger sitting in the rear seat opposite the driver. The researchers chose that seating arrangement because it maximizes the physical distance between the two people (although still less than the 6 feet recommended by the CDC). The models simulated the flow of air around and inside a car moving at 50 miles per hour, as well as the movement and concentration of aerosols from both the driver and passenger. Aerosols are tiny particles that can remain in the air for long periods of time. They are thought to be one way the SARS-CoV2 virus is transmitted, particularly in enclosed spaces.
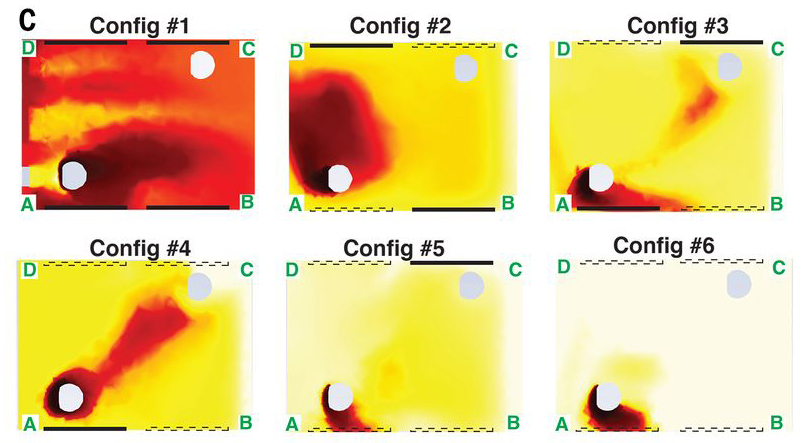
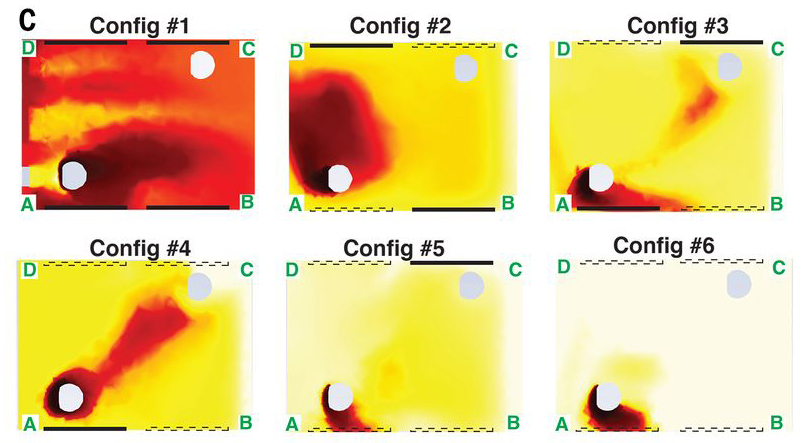
Part of the reason opening the windows is better in terms of aerosol transmission is because it increases the number of air changes per hour (ACH) inside the car, which helps reduce the overall aerosol concentration. But ACH was only part of the story, the researchers say. The study showed that different combinations of open windows created different air currents inside the car that could increase or decrease exposure to the remaining aerosols.
Due to the way air flows outside the car, the air pressure near the rear windows tends to be higher than the pressure on the front windows. As a result, air tends to enter the car through the rear windows and out the front windows. With all the windows open, this trend creates two more or less independent flows on either side of the cabin. Since the occupants in the simulations were seated on opposite sides of the cabin, very few particles end up being transferred between the two. The driver in this scenario is slightly more at risk than the passenger because the average airflow in the car goes from rear to front, but both occupants experience significantly less particle transfer than in any other scenario.
Simulations for scenarios in which some, but not all, windows are lowered have produced perhaps counterintuitive results. For example, you might expect opening windows directly next to each occupant to be the easiest way to reduce exposure. The simulations showed that while this configuration is better than the absence of lowered windows, it carries a greater exposure risk than lowering the window in front of each occupant.
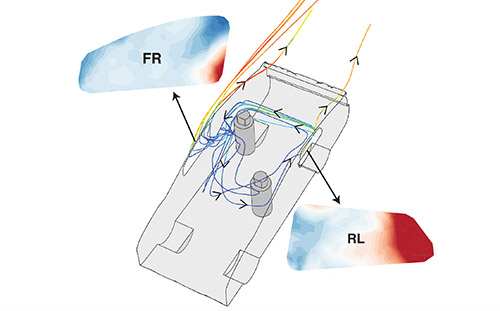
“When the windows in front of the occupants are open, you get a flow that enters the car behind the driver, goes through the cabin behind the passenger and then exits the front passenger side window,” said Kenny Breuer, an engineering professor at Brown. and a senior research author. “This scheme helps reduce cross-contamination between driver and passenger.”
It is important to note, the researchers say, that airflow adjustments do not replace the use of masks by both occupants inside a car. And the results are limited to potential exposure to persistent aerosols that may contain pathogens. The study did not model larger respiratory droplets or the risk of actually becoming infected with the virus.
However, the researchers say the study provides valuable new insight into air circulation patterns within a car’s cabin, something that had previously received little attention.
“This is the first study that we are aware of that has really looked at the microclimate inside a car,” Breuer said. “There have been some studies that have looked at the amount of external pollution that gets into a car or how long cigarette smoke stays in a car. But this is the first time anyone has looked at the airflow models in detail. “
The research grew out of a COVID-19 research task force set up in Brown to gather expertise from across the university to address very different aspects of the pandemic. Jeffrey Bailey, associate professor of pathology and laboratory medicine and co-author of the airflow study, leads the group. Bailey was impressed with how quickly the research came together, with Mathai suggesting the use of computer simulations that could be done while Brown’s lab research was on hiatus for the pandemic.
“This is really a great example of how different disciplines can come together quickly and produce valuable results,” Bailey said. “I spoke to Kenny briefly about this idea and within three or four days his team was already doing some preliminary tests. This is one of the great things about being in a place like Brown, where people are eager to collaborate and work across disciplines. “
.
[ad_2]
Source link